Abstract
Introduction:
Narcolepsy type 1 is accompanied by a selective loss of orexin/hypocretin (hcrt) neurons in the lateral hypothalamus caused by yet unknown mechanisms. Epidemiologic and genetic associations strongly suggest an immune-mediated pathogenesis of the disease.
Methods:
We compared specific T-cell reactivity to orexin/hcrt peptides in peripheral blood mononuclear cells of narcolepsy type 1 patients to healthy controls by a carboxyfluorescein succinimidyl ester proliferation assay. Orexin/hcrt-specific T-cell reactivity was also determined by cytokine (interferon gamma and granulocyte-macrophage colony-stimulating factor) analysis. Individuals were considered as responders if the cell division index of CD3+CD4+ T cells and both stimulation indices of cytokine secretion exceeded the cutoff 3. Additionally, T-cell reactivity to orexin/hcrt had to be confirmed by showing reactivity to single peptides present in different peptide pools.
Results:
Using these criteria, 3/15 patients (20%) and 0/13 controls (0%) showed orexin/hcrt-specific CD4+ T-cell proliferation (p = .2262). The heterogeneous reactivity pattern did not allow the identification of a preferential target epitope.
Conclusions:
A significant role of orexin/hcrt-specific T cells in narcolepsy type 1 patients could not be confirmed in this study. Further studies are needed to assess the exact role of CD4+ T cells and possible target antigens in narcolepsy type 1 patients.
Keywords: Narcolepsy type 1, autoimmune disease, orexin/hypocretin, CD4+ T-cell proliferation, HLA-DQB1*06:02.
Statement of Significance
Investigating T-cell-mediated autoimmunity in narcolepsy type 1 is very challenging and yielded conflicting results in the past. This is the first study to determine the rate of proliferating CD4+ T cells of patients with narcolepsy type 1 after stimulation with orexin/hypocretin peptides in vitro. In this setting, only a small subset of patients with a distinct T-cell proliferation could be identified. The exact role of CD4+ T cells in the pathogenesis of narcolepsy type 1 remains unclear and should be addressed in future studies.
INTRODUCTION
Narcolepsy is a lifelong chronic sleep disorder with excessive daytime sleepiness and disturbed nocturnal sleep. The disease is often accompanied by cataplexy (narcolepsy type 1), a sudden loss of muscle tone with retained consciousness triggered by emotions.1,2 Age of onset varies with peaks around the ages of 15 and 35 years3 and the prevalence lies between 25 and 50 per 100000 individuals.4
The etiology of narcolepsy type 1 is not known, but onset of clinical manifestation is related to a selective loss of approximately 90% orexin/hypocretin (hcrt)-producing neurons lying interspersed between melanin-concentrating hormone (MCH)–producing cells in the lateral hypothalamus. The fact that MCH-producing cells are spared suggests a highly selective mechanism of cell loss.5–7
Data from genetic, epidemiologic, and immunologic studies strongly suggest an immune-mediated pathogenesis of narcolepsy type 1. The genetic association with the human leukocyte antigen (HLA) class II allele DQB1*06:02,8–11 with more than 95% of patients with narcolepsy type 1 carrying this allele, as opposed to 12–38% HLA-DQB1*06:02-positive individuals in the general population,12–16 is much higher than in many well-established autoimmune diseases. More recently, further genes involved in immune modulation such as T-cell receptor alpha,17 OX40L,18 cathepsin H,18 and P2RY1119 were shown to be associated with narcolepsy in genome-wide association studies (GWAS), pointing towards a T-cell-mediated immune process.
The hypothesis of an immune-driven cause of the disease has recently been corroborated by reports of an increased incidence of narcolepsy in children following the 2009 H1N1 influenza virus pandemic in China20,21 and in children and adults after pandemic H1N1 vaccinations in Sweden, Finland, Ireland, UK, Norway, and France.22 Recently, antibodies reacting with a nucleoprotein of influenza virus, which is also present in the vaccine associated with narcolepsy, have been demonstrated to crossreact with orexin/hcrt receptor 2, further underscoring a possible autoimmune pathogenesis of the disease.23
Immunoglobulin G (IgG) from narcolepsy patients, but not from healthy controls, enhanced bladder parasympathetic cholinergic contractile responses, confirming a hypersensitivity to cholinergic stimulation in narcolepsy and suggesting the presence of a pathogenic autoantibody in patients.24 Attempts to identify possible target antigens involved in an autoantibody-mediated pathogenesis led to Tribbles homolog 2 (TRIB2). Antibodies against this intracellular antigen were found in 14–41% narcolepsy type 1 patients and only in 2–4% of controls, with higher antibody titers close to disease onset.25–27 Intra-cerebroventricular injection of pooled IgG from anti-TRIB2 antibody-positive narcolepsy patients into mice resulted in a decrease of neuronal and synaptic markers and of prepro-orexin in the lateral hypothalamus and caused behavioral changes resembling narcolepsy.28 However, results from a recent study using a similar approach in rats do not support the hypothesis that anti-TRIB2 antibodies cause the destruction of orexin/hcrt neurons.29 Potentially pathogenic antibodies against further yet unknown antigens were also shown to elicit different staining patterns in rat brain sections and to induce alterations of sleep patterns after passive IgG transfer.30
Taken together, despite many attempts to identify autoimmune causes for the pathogenesis of spontaneous (i.e. non vaccine/infection associated) narcolepsy type 1, definite evidence for an autoimmunity-driven mechanism is still lacking (recently reviewed).31 In particular, the role of T cells remains unclear.32,33 The majority of postmortem studies failed to detect microglial or T-cell infiltrations in affected hypothalamic areas of patients. However, since those studies were carried out often decades after disease onset, a possible role of immune cells at the time of disease onset cannot be excluded. Evidence from a case with concomitant Ma antibody-associated encephalitis showed gliosis and extensive CD8+ T-cell infiltrations in the hypothalamus 4 months after disease onset.34 In addition to the strong genetic association with HLA class II alleles suggesting an involvement of CD4+ T cells, to date, two studies reported an association with HLA class I alleles.35,36 Recently, using transgenic mice expressing hemagglutinin specifically in orexin/hcrt-producing neurons, it was shown that antigen-specific CD4+ and CD8+ T cells were able to infiltrate the hypothalamus and cause local inflammation, but only CD8+ T cells caused a selective loss of orexin/hcrt-producing neurons.37
In the present study, we investigated orexin/hcrt-specific CD4+ T-cell reactivity in peripheral blood mononuclear cells (PBMC) of patients with narcolepsy type 1 and healthy controls. For this purpose, we used a carboxyfluorescein succinimidyl ester (CFSE)–based proliferation assay that quantifies proliferating T cells and measured cytokine secretion after stimulation with a peptide library covering the full length pre-pro orexin/hcrt precursor protein.
METHODS AND MATERIALS
Study design and participants
In total, 15 patients with narcolepsy type 1 and 15 healthy controls were included in the study. Blood samples were drawn between 2013 and 2014 at the Clinical Department of Neurology, Innsbruck. For the primary evaluation, isolated PBMC were used immediately for subsequent experiments, without cryopreservation. Initially, cells of some individuals did not proliferate in response to positive control peptides, and results of those stimulations were considered unreliable. Therefore, reassessments were made from frozen PBMC of these individuals (patients #7, #9, and #10, and controls #3, #4, #10, and #14), yielding a clear proliferation in response to positive control peptides. All patients were seen by experts in sleep medicine (B.H., A.S., T.M.) and fulfilled the diagnostic criteria of narcolepsy type 12 (or ICSD-2,38 since all patients were diagnosed before 2014). The present study was approved by the Ethical Committee of the Medical University of Innsbruck (study number UN4966 322/4.10), and all patients and controls gave written informed consent to the study protocol. For patients younger than 18 years of age, written informed consent was sought from a parent or legal guardian. In total, 2 minors were enrolled in the study and written informed consent was sought from a parent on their behalf.
Proliferation assay
Whole blood was collected in EDTA containing Monovette® collection tubes (Sarstedt, Nuembrecht, Germany). PBMC were isolated using Ficoll gradient reagent (Sigma-Aldrich, St. Louis, MO, USA) and immediately used for subsequent experiments or frozen for later analyses. At a density of 2 × 107 cells per milliliter, isolated PBMC were stained with 0.4 µM CFSE (Life Technologies, Carlsbad, CA, USA) following the manufacturer’s instructions with minor modifications. Briefly, PBMC were stained with CFSE diluted in PBS (Sigma-Aldrich) for 5 min at 37°C. The reaction was stopped by adding RPMI-1640 growth medium containing 10% FCS (both Life Technologies). The cell suspension was placed on ice for 10 min, and after one further washing step with RPMI-1640 containing 10% FCS, followed by one washing step with RPMI-1640 without FCS, the cells were cultivated in X-Vivo 15 growth medium (Lonza, Basel, Switzerland). For the expansion of antigen-specific T cells, PBMC were exposed to orexin/hcrt peptide pools covering the full length protein (Peptides & Elephants, Potsdam, Germany). A peptide library of overlapping 15-mer peptides and two 13-mer peptides (orexin/hcrt1-13 and orexin/hcrt45-57 that were included due to their predicted high binding affinity for HLA-DQB1*06:02)39 was generated, and each peptide (10 µg/mL) was contained in 2 different peptide pools (Table 1). This setup has the following advantages: (1) the number of total reactions is reduced and (2) each peptide is contained in exactly 2 peptide pools, which allows the identification of specific epitopes involved in possible immune reactions. As controls, a tetanus toxin (TTX) pool (Peptides & Elephants) and a pool of myelin peptides (MBP13–32, MBP83–99, MBP111–129, MBP146–170, MOG1–20, MOG35–55, PLP139–154; 10 µg/mL; Bachem AG, Bubendorf, Switzerland)40 were used. As vehicle control, dimethyl sulfoxide (Sigma-Aldrich) was used. Cells were seeded at a density of 2 × 105 cells per 200 µL in tissue culture test plates 96U (TPP, Trasadingen, Switzerland), each 6 wells per condition. After 48 h 50 µL of supernatant were replaced by fresh culture medium in each well and stored at −80°C for cytokine analysis. After 8 days, cell were restimulated with either peptide pools (10 µg/mL per peptide) or vehicle control, and 100 µL of the supernatant were replaced with fresh medium containing 20 U/mL IL-2 (Peprotech, Hamburg, Germany) and stored at −80°C. Three days later, PBMC were harvested and analyzed by flow cytometry. To determine the proliferation of T cells, PBMC were stained with CD3, CD4, and CD45RO antibodies (all BD Bioscience, Franklin Lakes, NJ, USA) and analyzed on an Accuri C6 flow cytometer (BD Bioscience). For analysis of a positive T-cell proliferation response, the cell division index (CDI) was calculated as follows:
Table 1.
Orexin/hcrt Peptide Pools Used for Stimulation of PBMC.
| Pool 5 | Pool 6 | Pool 7 | Pool 8 | |
|---|---|---|---|---|
| Pool 1 | Orexin/hcrt1–13 MNLPSTKVSWAAV |
Orexin/hcrt45–57 CSCRLYELLHGAG |
Orexin/hcrt1–15 MNLPSTKVSWAAVTL |
Orexin/hcrt11–25 AAVTLLLLLLLLPPA |
| Pool 2 | Orexin/hcrt21–35 LLPPALLSSGAAAQP |
Orexin/hcrt31–45 AAAQPLPDCCRQKTC |
Orexin/hcrt41–55 RQKTCSCRLYELLHG |
Orexin/hcrt51–65 ELLHGAGNHAAGILT |
| Pool 3 | Orexin/hcrt61–75 AGILTLGKRRSGPPG |
Orexin/hcrt71–85 SGPPGLQGRLQRLLQ |
Orexin/hcrt81–95 QRLLQASGNHAAGIL |
Orexin/hcrt91–105 AAGILTMGRRAGAEP |
| Pool 4 | Orexin/hcrt101–115 AGAEPAPRPCLGRRC |
Orexin/hcrt111–125 LGRRCSAPAAASVAP |
Orexin/hcrt117–131 APAAASVAPGGQSGI |
A peptide library from full length orexin/hcrt was created. Pools 1, 2, 3, 5, 6, and 7 contained each 4 orexin/hcrt peptides, pools 4 and 8 contained each 3 orexin/hcrt peptides at a concentration of 10 µg/mL per peptide. Each peptide was contained in 2 different pools.
Hcrt = hypocretin. PBMC = peripheral blood mononuclear cells.
A CDI ≥ 3 was considered as significant proliferation.
Interferon gamma and granulocyte-macrophage colony-stimulating factor levels
Cell culture supernatants from 48 h, days 8 and 11 were stored at −80°C until use. Interferon gamma (IFN-γ) and granulocyte-macrophage colony-stimulating factor (GM-CSF) levels in the supernatants were determined by commercially available Luminex-based ProcartaPlex Immunoassays (48 h; eBioscience, San Diego, CA, USA) or enzyme-linked immunosorbent assay kits (days 8 and 11; BioLegend, San Diego, CA, USA). Stimulation indices (SIs) and cutoff values were calculated as described for CDI.
Genomic HLA typing
To determine the frequency of the HLA-DQB1*06:02 allele of patients and controls from genomic DNA the Olerup SSP® DQB1*06:02, DQA1*01:02 Typing Kit (Vienna, Austria) was used.
Statistical analysis
Statistical analysis was done using GraphPad Prism 7 (GraphPad, San Diego, CA, USA). Between-group comparisons were performed with Kruskal–Wallis test, Mann–Whitney U test, Fisher’s exact test, and Dunn’s multiple comparison post-hoc test when appropriate. Correlation of parameters was analyzed with Spearman’s non-parametric correlation. Statistical significance was defined as 2-sided p-value < 0.05.
RESULTS
Frequency of the HLA-DQB1*06:02 allele in patients and controls
Demographic data of all patients and controls included in the study are shown in Table 2. All 15 patients with narcolepsy type 1 were positive for the HLA-DQB1*06:02 allele (100%) and 2/10 healthy controls were HLA-DQB1*06:02 positive (20%), consistent with the reported distribution of this allele in patients and controls.8,9,12–16 In order to control for a possible confounding effect of the HLA-DQB1*06:02 allele, we increased the number of HLA-DQB1*06:02-positive healthy controls by selectively including 5 further healthy controls with the HLA-DQB1*06:02 allele (#11–15), allowing subgroup analyses of HLA-DQB1*06:02-positive and negative controls.
Table 2.
Demographic Data and CD3+ T-cell Proliferation to Orexin/hcrt Peptide Pools of All Patients and Controls.
| Patients | Gender/age† | HLA-DQB1*06:02 positive | Disease duration† | H1N1 vaccination | CD4+ T-cell reactivity to TTX control peptides | CD4+ T-cell reactivity to orexin/ hcrt pool(s) | CD4− T-cell reactivity to orexin/ hcrt pool(s) |
|---|---|---|---|---|---|---|---|
| P1 | M 55 | Yes | 28 | Not known | Yes | 5 | No |
| P2 | M 40 | Yes | 10 | No | Yes | No | No |
| P3 | M 31 | Yes | 5 | Not known | Yes | No | No |
| P4 | M 45 | Yes | 25 | No | Yes | No | No |
| P5 | F 57 | Yes | 9 | No | Yes | 7 | 7 |
| P6 | F 68 | Yes | 18 | No | Yes | 1, 7, 8 | 1, 7, 8 |
| P7 | M 38 | Yes | 2 | No | Yes | 5 | No |
| P8 | F 62 | Yes | 46 | No | Yes | No | No |
| P9 | M 14 | Yes | 1 | No | Yes | 4# | No |
| P10 | M 18 | Yes | 8 | No | Yes | 2*, 6 | No |
| P11 | F 12 | Yes | 3 | Not known | Yes | No | No |
| P12 | M 56 | Yes | 24 | Not known | Yes | No | No |
| P13 | F 38 | Yes | 15 | No | Yes | 2, 6 | 2, 6, 8# |
| P14 | M 34 | Yes | 10 | Not known | Yes | No | 3# |
| P15 | F 19 | Yes | 6 | No | Yes | No | No |
| M:F | 9:6 | 15/15 | |||||
| Median (range)† | 39.1 (12–68) | 10 (1–46) | |||||
| Controls | Gender/age | HLA-DQB1*06:02 | |||||
| C1 | F 27 | No | n/a | No | Yes | No | No |
| C2 | M 31 | No | n/a | No | Yes | No | No |
| C3 | M 48 | No | n/a | No | Yes | No | No |
| C4 | M 52 | No | n/a | No | Yes | 2#,6#,7# | 6# |
| C5 | M 48 | Yes | n/a | No | No | No | No |
| C6 | M 38 | No | n/a | No | Yes* | No | No |
| C7 | F 60 | No | n/a | No | No | No | No |
| C8 | M 60 | No | n/a | No | Yes | No | No |
| C9 | F 61 | Yes | n/a | No | Yes | No | No |
| C10 | M 21 | No | n/a | No | Yes | No | No |
| C11 | F 29 | Yes | n/a | No | Yes | No | No |
| C12 | F 27 | Yes | n/a | No | Yes | 4#, 5# | 5# |
| C13 | M 32 | yes | n/a | No | Yes | No | No |
| C14 | F 35 | Yes | n/a | No | Yes | No | No |
| C15 | F 25 | Yes | n/a | No | Yes | No | No |
| M:F | 8:7 | 7/15 | |||||
| Median (range)† | 39.6 (21–61) | n/a |
†Years; #CD4+ T-cell proliferation was not confirmed by secretion of both cytokines. *CD4+ T-cell reactivity had detected a CDI of 2.94, which was marginally below the cutoff (3) but clearly elevated SI ≥3 of IFN-γ and GM-CSF secretion.
CDI = cell division index. GM-CSF = granulocyte-macrophage colony-stimulating factor. hcrt = hypocretin. IFN-γ = interferon gamma. n/a = not applicable. PBMC = peripheral blood mononuclear cells. SI = stimulation index.
CD4+ T-cell proliferation to orexin/hcrt and control peptides
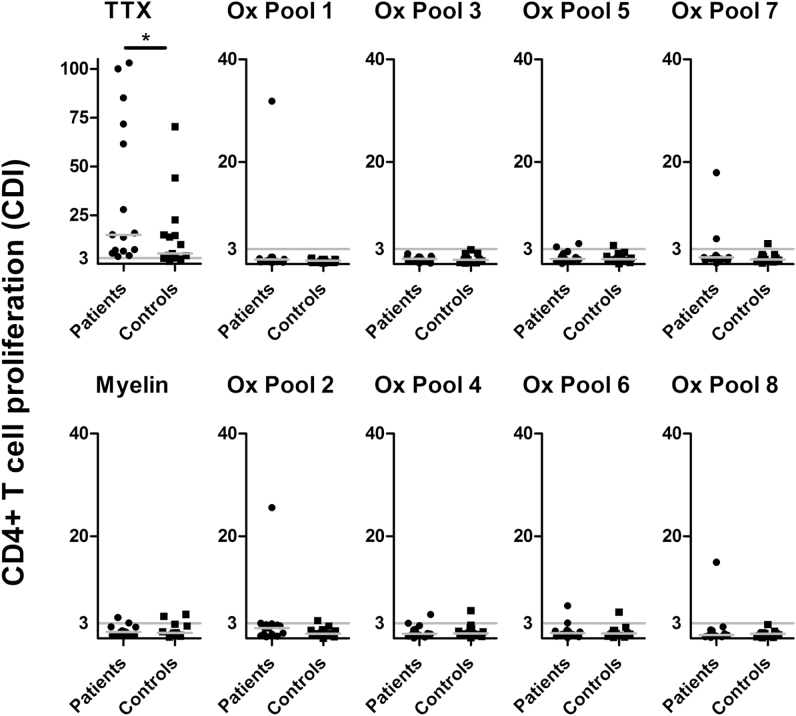
The gating strategy for identification of CD3+CD4+CFSE− cells is shown in Figure 1. CD4+ T-cell proliferation in response to the control peptides TTX was higher compared to proliferation in response to orexin/hcrt peptide pools across all groups (p < .0001). CD4+ T-cell proliferation to TTX was higher in patients compared to controls (p < .05) but did not reach statistical significance when comparing HLA-DQB1*06:02-positive patients and controls only. No further significant group-specific differences in CD4+ T-cell proliferation were observed in response to myelin or orexin/hcrt peptide pools (Figure 2).
Figure 1.
Gating strategy for identification of proliferated CD3+ T cells.
PBMC stimulated with orexin/hcrt or control peptides after 11 days in culture were analyzed. Gating of lymphocytes (A), CD3+ cells (B), CD4+ and CD4− T cells (C) is shown. (D–F) Gating of proliferated CFSE− T cells. This example shows proliferated T cells to the vehicle control (D), in response to TTX peptides (E) and orexin/hcrt pool 6 of patient #13 (F).
CFSE = carboxyfluorescein succinimidyl ester. FSC = forward scatter. PBMC = peripheral blood mononuclear cells. SSC = side scatter. TTX = tetanus toxin.
Figure 2.
TTX, myelin and orexin/hcrt-specific CD4+ T-cell proliferation in narcolepsy patients and controls.
PBMC from patients with narcolepsy type 1 and healthy controls were analyzed by CFSE proliferation assay in response to TTX, myelin, and orexin/hcrt peptide pools (Table 1) after 11 days of stimulation. CD3+CD4+CFSE− cells were quantified by calculation of the CDI. Fifteen patients with narcolepsy type 1 and 15 healthy controls were analyzed. The cutoff CDI (≥3) is indicated by horizontal gray lines. Medians are shown by horizontal gray bars. Between-group comparisons were calculated by Mann–Whitney U test. *p < .05.
CDI = cell division index. CFSE = carboxyfluorescein succinimidyl ester. Ox Pool 1–8 = orexin/hcrt peptide pools. PBMC = peripheral blood mononuclear cells. TTX = tetanus toxin.
A positive CD4+ CDI (≥3) to the TTX control peptides was observed in 15/15 (100%) patients with narcolepsy type 1, in 6/7 (86%) HLA-DQB1*06:02-positive healthy controls and in 7/8 (88%) HLA-DQB1*06:02-negative healthy controls. Individuals who did not respond to TTX control peptides (i.e. 2 healthy controls) were excluded from further statistical analysis when using Fisher’s exact test. Significant CD4+ T-cell responses to any orexin/hcrt peptide pool were observed in 7/15 (47%) patients and in 2/13 (15%) healthy controls, without reaching statistical significance between the groups (p = .1145; Figure 3, Table 2). Four of 9 responders were female and 5 male. Among the non-responders, 8 were female and 11 male. We did not find significant differences related to gender. The vast majority of proliferating CD4+ T cells was positive for the memory T-cell marker CD45RO compared to CD4+ T cells from samples not showing a distinct proliferation (98.0% vs. 81.7% (patients) and 95.7% vs. 78.1% (controls); p < .0001; Figure S1 in supplemental material). Significant proliferation in response to myelin peptides was seen in 2 patients and 2 healthy controls.
Figure 3.
T-cell proliferation and cytokine secretion in response to TTX, myelin, and orexin/hcrt peptide pools. PBMC of patients with narcolepsy type 1 (n = 15) and of healthy controls (n = 15) were stimulated with respective peptide pools for 11 days. Heat maps indicate CDI of CD3+CD4+ and CD3+CD4− cells and SI of IFN-γ and GM-CSF. The cutoff CDI and SI (≥3) is indicated in white, values below in blue and above in red. Missing values are shown in gray. Note that C#5 and C#7 were excluded due to low CD4+ T-cell proliferation (CDI < 3).
C#1–15 = (healthy) controls. CDI = cell division index. DMSO = dimethyl sulfoxide (vehicle control). GM-CSF = granulocyte-macrophage colony-stimulating factor. IFN-γ = interferon gamma. OxPool1-8 = orexin/hcrt peptide pools. P#1–15 = (narcolepsy type 1) patients. PBMC = peripheral blood mononuclear cells. SI = stimulation index. TTX = tetanus toxin (positive control).
There were no statistically significant differences in subgroup analyses between HLA-DQB1*06:02-positive and negative healthy controls.
IFN-γ and GM-CSF secretion after orexin/hcrt stimulation
To complement the findings of the proliferation responses (CDI), we measured the levels of cytokines after stimulation with peptides at 48 h, day 8 (before restimulation) and day 11. The IFN-γ and GM-CSF concentrations in cell culture supernatants after 48 h and after 8 days of culture were frequently below the detection limit. At 48 h, 38/40 (95%) tested samples were below detection limits, missing 2/4 (50%) control reactions to TTX, and all samples from patient #6 who showed a clear CD4+ T-cell proliferation to orexin/hcrt pools 1, 7, and 8 in the CFSE-based proliferation assay and cytokine secretion after 11 days. At 8 days still >50% of IFN-γ and GM-CSF levels were below detection limits and therefore considered as unreliable (data not shown). After 11 days, 7% and 13% of IFN-γ and GM-CSF levels, respectively, were below detection limits. SI of IFN-γ and GM-CSF levels after 11 days of culture correlated well with CDI in the proliferation assay: 0.73 [95% confidence interval (CI): 0.67–0.78] and 0.71 (95% CI: 0.65–0.76), respectively (Spearman ρ; p < .0001). As can be seen in Figure 3, SI of cytokine levels exceeded the cutoff (≥3) more often than the above described CDI in patients and controls.
Identification of orexin/hcrt epitopes eliciting an immune response
The orexin/hcrt peptide pools consisting of a peptide library derived from the full length orexin/hcrt protein were designed to be able to identify 15-mer peptides yielding a possible immune response, since each peptide was contained in 2 pools (Table 1). Four patients (#1, #5, #7, and #9) showed CD4+ T-cell proliferation to each one peptide pool; therefore, no peptide-specific proliferation could be confirmed in these patients. However, 3 patients (#6, #10, and #13) showed proliferation to multiple peptide pools, and this proliferation was also confirmed by IFN-γ and GM-CSF secretion: CD4+ T cells of patient #6 reacted to pools 1, 7, and 8, and CD4+ T cells of patients #10 and #13 to pools 2 and 6, leading to orexin/hcrt1–15 and orexin/hcrt11–25 (patient #6), and orexin/hcrt31–45 (patients #10 and #13) as possible target epitopes. Thus, the CD4+ T-cell proliferation of narcolepsy type 1 patients follows a heterogeneous pattern but is restricted to the N-terminal region of orexin/hcrt.
In contrast, CD4+ T-cell proliferation of 2 healthy controls (#4: pools 2, 6, and 7; #12: pools 4 and 5) was not confirmed by IFN-γ and GM-CSF secretion.
Using these stringent criteria, only 3 of 15 (20%) patients had a significant response to orexin/hcrt peptides as opposed to 0 of 13 (0%) healthy controls (p = .2262).
Orexin/hcrt-specific CD3+CD4− cell proliferation
Although we cannot certainly identify CD8+ T cells with this setting, we further analyzed the population of CD3+CD4– cells, which comprises cytotoxic CD8+ T cells, CD3+ natural killer (NK) T cells and γδ T cells. The gating strategy for identification of CD3+CD4−CFSE− cells is shown in Figure 1. As observed for CD3+CD4+ T cells, CD3+CD4− cell proliferation in response to the control peptides TTX was higher compared to proliferation in response to orexin/hcrt peptide pools across all groups (p < .0001; Figure S2 in supplemental material). No significant group-specific differences in CD3+CD4− cell proliferation were observed in response to orexin/hcrt peptide pools. A CDI ≥ 3 to any orexin/hcrt peptide was observed in 4/15 (27%) patients and 2/13 (15%) healthy controls (p = .6546). CD3+CD4− cell reactivity largely overlapped with CD3+CD4+ T-cell reactivity specific for orexin/hcrt peptides (Figure 3 and Table 2). There were only 2 responses of CD3+CD4− cells that were not observed for CD3+CD4+ T cells, which were however also not detectable by cytokine secretion (patient #13 to orexin/hcrt pool 8 and patient #14 to orexin/hcrt pool 3).
DISCUSSION
In the present study, we found some patients with narcolepsy type 1 (7/15; 47%) showing a peripheral CD4+ T-cell reactivity in response to orexin/hcrt peptides, while orexin/hcrt-specific responses were observed in 2/13 (15%) healthy controls. However, when considering only those individuals with specific T-cell reactivity to single orexin/hcrt peptides, confirmed by reactivity to different pools containing the same peptide, and cytokine secretion, only 3/15 (20%) patients and 0/13 (0%) healthy controls had a positive response. The difference between patients and controls did not reach statistical significance, which is in line with a recent study reporting no significant difference in IFN-γ production in blood of patients in response to orexin/hcrt B.41 Furthermore, no specific epitope could be identified, although the experimental setup was designed to enable the identification of 15-mer target peptides. We used very stringent criteria to exclude false positives, i.e. individuals having T-cell reactivity to only one of two peptide pools, or if the T-cell proliferation was not confirmed by cytokine secretion.
It can be speculated that a putative epitope eliciting T-cell response in our patients is located rather in the N-terminal part of the full length protein (orexin/hcrt1–60), since stimulation with peptide pools containing exclusively C-terminal epitopes (orexin/hcrt61–131; pools 3 and 4) did not result in a positive CD4+ T-cell proliferation in any of the patients, with the exception of patient #9 responding to orexin/hcrt pool 4, which was however not confirmed by cytokine secretion. The N-terminal part of orexin/hcrt contains the signal peptide (orexin/hcrt1–33) and the secreted orexin/hcrt A (orexin/hcrt34–66).42,43 One interesting observation was the higher proliferation to the TTX control peptides in narcolepsy type 1 patients compared to healthy controls, reaching significance for CD4+ T cells. However, the difference was not significant anymore when considering only DQB1*06:02-positive controls. Thus, the HLA class II allele is an important determinant of the response to TTX, as was previously demonstrated for different vaccines.44,45 Still, proliferation was more pronounced in narcolepsy patients. Thus, besides the HLA class II allele, additional factors that can modulate T-cell reactivity to TTX might differ between narcolepsy type 1 patients and healthy controls. This is in line with results from GWAS in narcolepsy pointing towards genes involved in immune modulation of T cells,17–19 although this is purely speculative based on the data from our study.
Experimental procedure and analysis of data used in this study were carefully selected to keep very stringent readout criteria, combining different methods to determine peptide-specific T-cell response: (1) dilution of CFSE-stained CD4+ cells, which is a direct way to determine cell proliferation; (2) secretion of IFN-γ; and (3) GM-CSF to the cell culture supernatant. The combination of both readouts, i.e. T-cell proliferation and cytokine secretion strongly increases the validity of the results. Furthermore, we used mainly freshly isolated PBMC to improve the quality of our analysis.
Our study also has limitations. First, the number of patients and controls was small (n = 15). However, an a priori sample size calculation revealed that this number is sufficient to detect a biologically relevant difference of 50% with a statistical power of 80% and 5% alpha. Furthermore, the precursor frequency of orexin/hcrt-specific T cells might be too low for the assays used in the study. Overall, we used 1.2 × 106 PBMC for each condition, which is in line with reported precursor frequencies for auto-antigens,46 but we cannot exclude that these are very much lower in narcolepsy type 1 patients. In our study, the reactivity to the TTX-positive control peptides was absent in two of the healthy controls. We therefore considered cells of those individuals as not sufficiently responsive to antigen-specific proliferation and excluded them from further statistical analysis when using Fisher’s exact test.
The median disease duration of the narcolepsy patients investigated in our study was 10 years, and most of the patients had the disease for 10 or more years. This is a general issue since diagnosis of narcolepsy is frequently made several years after the actual onset of the disease, with a reported mean delay of 15 years or more.47 The 3 patients with a positive T-cell response had a mean disease duration of 14 years (range 8–18). In contrast, none of the 4 patients with a disease duration of 5 years or less showed a convincing orexin/hcrt-specific T-cell reactivity. Thus, T-cell reactivity to orexin/hcrt might rather reflect a secondary process than an initial event in narcolepsy type 1.
Only 28% of the population aged 15–59 years and 40% of the population older than 60 years are vaccinated against influenza H1N1 in Austria,48 which is far below the European Union target (75%) and several other European Union Member States.49 In the present study, to our knowledge, none of the 15 patients was vaccinated against H1N1. Therefore, the cases described here represent a cohort of spontaneous narcolepsy type 1 patients (as opposed to patients that developed the disease after H1N1 vaccination), and it is not possible to conclude any possible effects of H1N1 vaccinations on the parameters investigated here.
Finally, the nature of proliferating CD3+CD4− cells (comprising CD8+, CD3+ NKT cells and γδ T cells) observed in some individuals could not be further specified since the main focus of this study were CD4+ T-cell responses. Due to increasing evidence for a contribution of CD8+ T cells in the pathogenesis of narcolepsy,35–37 a more specific analysis of CD8+ T-cell reactivity is warranted in future studies.
Overall, we conclude that orexin/hcrt-specific T-cell responses are elevated in some but not significantly more frequently in patients with narcolepsy type 1 compared to healthy controls. Our data do not suggest that orexin/hcrt is a predominant target antigen for T cells in narcolepsy type 1 patients. However, the observed tendency seen here does not exclude an autoimmune contribution and adds one further aspect to the myriad of ambiguous data on the topic. Similarly, recent studies investigating cytokine profiles in serum or CSF of narcolepsy patients yielded contradicting data detecting either differentially regulated cytokines in narcolepsy50–52 or no significant group specific differences.53
The biological relevance of the observed T-cell reactivity to orexin/hcrt in the 3 positively tested patients remains unclear, and no single target peptide could be identified. Important questions as the frequency of orexin/hcrt-specific T-cell responses at disease onset or the influence of such T-cell responses on phenotype and disease course should be analyzed in studies with larger sample sizes and longitudinally repeated sampling.
SUPPLEMENTAL MATERIAL
Supplementary data are available at SLEEPJ online.
FUNDING
This study was supported by the Fonds zur Förderung der wissenschaftlichen Forschung, Austria (FWF graduate program W1206 SPIN, MeR and MaR). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
CLINICAL TRIAL
N/A
DISCLOSURES
The authors have no conflicts of interest.
Supplementary Material
REFERENCES
- 1. Dauvilliers Y, Arnulf I, Mignot E. Narcolepsy with cataplexy. Lancet. 2007; 369(9560): 499–511. [DOI] [PubMed] [Google Scholar]
- 2. American Academy of Sleep Medicine. International Classification of Sleep Disorders, 3rd ed(ICSD-3). Darien, IL; 2014. [Google Scholar]
- 3. Dauvilliers Y, Montplaisir J, Molinari N, et al. Age at onset of narcolepsy in two large populations of patients in France and Quebec. Neurology. 2001; 57(11): 2029–2033. [DOI] [PubMed] [Google Scholar]
- 4. Longstreth WT, Jr, Koepsell TD, Ton TG, Hendrickson AF, van Belle G. The epidemiology of narcolepsy. Sleep. 2007; 30(1): 13–26. [DOI] [PubMed] [Google Scholar]
- 5. Thannickal TC, Moore RY, Nienhuis R, et al. Reduced number of hypocretin neurons in human narcolepsy. Neuron. 2000; 27(3): 469–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thannickal TC, Nienhuis R, Siegel JM. Localized loss of hypocretin (orexin) cells in narcolepsy without cataplexy. Sleep. 2009; 32(8): 993–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thannickal TC, Siegel JM, Nienhuis R, Moore RY. Pattern of hypocretin (orexin) soma and axon loss, and gliosis, in human narcolepsy. Brain Pathol. 2003; 13(3): 340–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mignot E, Lin X, Arrigoni J, et al. DQB1*0602 and DQA1*0102 (DQ1) are better markers than DR2 for narcolepsy in Caucasian and black Americans. Sleep. 1994; 17(8): S60–S67. [DOI] [PubMed] [Google Scholar]
- 9. Mignot E. Genetics of narcolepsy and other sleep disorders. Am J Hum Genet. 1997; 60(6): 1289–1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Juji T, Satake M, Honda Y, Doi Y. HLA antigens in Japanese patients with narcolepsy. All the patients were DR2 positive. Tissue Antigens. 1984; 24(5): 316–319. [DOI] [PubMed] [Google Scholar]
- 11. Langdon N, Welsh KI, van Dam M, Vaughan RW, Parkes D. Genetic markers in narcolepsy. Lancet. 1984; 2(8413): 1178–1180. [DOI] [PubMed] [Google Scholar]
- 12. Mignot E, Lin L, Rogers W, et al. Complex HLA-DR and -DQ interactions confer risk of narcolepsy-cataplexy in three ethnic groups. Am J Hum Genet. 2001; 68(3): 686–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mignot E. Genetic and familial aspects of narcolepsy. Neurology. 1998; 50(2): S16–S22. [DOI] [PubMed] [Google Scholar]
- 14. Mignot E, Lammers GJ, Ripley B, et al. The role of cerebrospinal fluid hypocretin measurement in the diagnosis of narcolepsy and other hypersomnias. Arch Neurol. 2002; 59(10): 1553–1562. [DOI] [PubMed] [Google Scholar]
- 15. Rogers AE, Meehan J, Guilleminault C, Grumet FC, Mignot E. HLA DR15 (DR2) and DQB1*0602 typing studies in 188 narcoleptic patients with cataplexy. Neurology. 1997; 48(6): 1550–1556. [DOI] [PubMed] [Google Scholar]
- 16. Tafti M, Hor H, Dauvilliers Y, et al. DQB1 locus alone explains most of the risk and protection in narcolepsy with cataplexy in Europe. Sleep. 2014; 37(1): 19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hallmayer J, Faraco J, Lin L, et al. Narcolepsy is strongly associated with the T-cell receptor alpha locus. Nat Genet. 2009; 41(6): 708–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Faraco J, Lin L, Kornum BR, et al. ImmunoChip study implicates antigen presentation to T cells in narcolepsy. PLoS Genet. 2013; 9(2): e1003270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kornum BR, Kawashima M, Faraco J, et al. Common variants in P2RY11 are associated with narcolepsy. Nat Genet. 2011; 43(1): 66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Han F, Lin L, Warby SC, et al. Narcolepsy onset is seasonal and increased following the 2009 H1N1 pandemic in China. Ann Neurol. 2011; 70(3): 410–417. [DOI] [PubMed] [Google Scholar]
- 21. Han F, Lin L, Li J, Dong XS, Mignot E. Decreased incidence of childhood narcolepsy 2 years after the 2009 H1N1 winter flu pandemic. Ann Neurol. 2013; 73(4): 560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ahmed SS, Schur PH, MacDonald NE, Steinman L. Narcolepsy, 2009 A(H1N1) pandemic influenza, and pandemic influenza vaccinations: what is known and unknown about the neurological disorder, the role for autoimmunity, and vaccine adjuvants. J Autoimmun. 2014; 50: 1–11. [DOI] [PubMed] [Google Scholar]
- 23. Ahmed SS, Volkmuth W, Duca J, et al. Antibodies to influenza nucleoprotein cross-react with human hypocretin receptor 2. Sci Transl Med. 2015; 7(294): 294ra105. [DOI] [PubMed] [Google Scholar]
- 24. Smith AJ, Jackson MW, Neufing P, McEvoy RD, Gordon TP. A functional autoantibody in narcolepsy. Lancet. 2004; 364(9451): 2122–2124. [DOI] [PubMed] [Google Scholar]
- 25. Cvetkovic-Lopes V, Bayer L, Dorsaz S, et al. Elevated Tribbles homolog 2-specific antibody levels in narcolepsy patients. J Clin Invest. 2010; 120(3): 713–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Toyoda H, Tanaka S, Miyagawa T, Honda Y, Tokunaga K, Honda M. Anti-Tribbles homolog 2 autoantibodies in Japanese patients with narcolepsy. Sleep. 2010; 33(7): 875–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kawashima M, Lin L, Tanaka S, et al. Anti-Tribbles homolog 2 (TRIB2) autoantibodies in narcolepsy are associated with recent onset of cataplexy. Sleep. 2010; 33(7): 869–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Katzav A, Arango MT, Kivity S, et al. Passive transfer of narcolepsy: anti-TRIB2 autoantibody positive patient IgG causes hypothalamic orexin neuron loss and sleep attacks in mice. J Autoimmun. 2013; 45: 24–30. [DOI] [PubMed] [Google Scholar]
- 29. Tanaka S, Honda Y, Honda M, Yamada H, Honda K, Kodama T. Anti-tribbles pseudokinase 2 (TRIB2)-immunization modulates HYPOCRETIN/OREXIN neuronal functions. Sleep 2016. Sep 9. pii: sp-00219-16 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 30. Bergman P, Adori C, Vas S, et al. Narcolepsy patients have antibodies that stain distinct cell populations in rat brain and influence sleep patterns. Proc Natl Acad Sci USA. 2014; 111(35): E3735–E3744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Liblau RS, Vassalli A, Seifinejad A, Tafti M. Hypocretin (orexin) biology and the pathophysiology of narcolepsy with cataplexy. Lancet Neurol. 2015; 14(3): 318–328. [DOI] [PubMed] [Google Scholar]
- 32. De la Herran-Arita AK, Kornum BR, Mahlios J, et al. Retraction of the research article: “CD4(+) T cell autoimmunity to hypocretin/orexin and cross-reactivity to a 2009 H1N1 influenza A epitope in narcolepsy”. Sci Transl Med 2014; 6: 247rt1. [DOI] [PubMed] [Google Scholar]
- 33. Partinen M, Kornum BR, Plazzi G, Jennum P, Julkunen I, Vaarala O. Does autoreactivity have a role in narcolepsy? Lancet Neurol. 2014; 13(11): 1072–1073. [DOI] [PubMed] [Google Scholar]
- 34. Dauvilliers Y, Bauer J, Rigau V, et al. Hypothalamic immunopathology in anti-Ma-associated diencephalitis with narcolepsy-cataplexy. JAMA Neurol. 2013; 70(10): 1305–1310. [DOI] [PubMed] [Google Scholar]
- 35. Ollila HM, Ravel JM, Han F, et al. HLA-DPB1 and HLA class I confer risk of and protection from narcolepsy. Am J Hum Genet. 2015; 96(1): 136–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tafti M, Lammers GJ, Dauvilliers Y, et al. Narcolepsy-associated HLA class I alleles implicate cell-mediated cytotoxicity. Sleep. 2016; 39(3): 581–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bernard-Valnet R, Yshii L, Quériault C, et al. CD8 T cell-mediated killing of orexinergic neurons induces a narcolepsy-like phenotype in mice. Proc Natl Acad Sci USA. 2016; 113(39): 10956–10961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. American Academy of Sleep Medicine. The International Classification of Sleep Disorders, 2nd ed(ICSD-2) Westchester, IL; 2005. [Google Scholar]
- 39. Siebold C, Hansen BE, Wyer JR, et al. Crystal structure of HLA-DQ0602 that protects against type 1 diabetes and confers strong susceptibility to narcolepsy. Proc Natl Acad Sci USA. 2004; 101(7): 1999–2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lutterotti A, Yousef S, Sputtek A, et al. Antigen-specific tolerance by autologous myelin peptide-coupled cells: a phase 1 trial in multiple sclerosis. Sci Transl Med. 2013; 5(188): 188ra75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ambati A, Poiret T, Svahn BM, et al. Increased beta-haemolytic group A streptococcal M6 serotype and streptodornase B-specific cellular immune responses in Swedish narcolepsy cases. J Intern Med. 2015; 278(3): 264–276. [DOI] [PubMed] [Google Scholar]
- 42. Sakurai T, Moriguchi T, Furuya K, et al. Structure and function of human prepro-orexin gene. J Biol Chem. 1999; 274(25): 17771–17776. [DOI] [PubMed] [Google Scholar]
- 43. Lee JH, Bang E, Chae KJ, Kim JY, Lee DW, Lee W. Solution structure of a new hypothalamic neuropeptide, human hypocretin-2/orexin-B. Eur J Biochem. 1999; 266(3): 831–839. [DOI] [PubMed] [Google Scholar]
- 44. Yucesoy B, Talzhanov Y, Johnson VJ, et al. Genetic variants within the MHC region are associated with immune responsiveness to childhood vaccinations. Vaccine. 2013; 31(46): 5381–5391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Posteraro B, Pastorino R, Di Giannantonio P, et al. The link between genetic variation and variability in vaccine responses: systematic review and meta-analyses. Vaccine. 2014; 32(15): 1661–1669. [DOI] [PubMed] [Google Scholar]
- 46. Bielekova B, Goodwin B, Richert N, et al. Encephalitogenic potential of the myelin basic protein peptide (amino acids 83-99) in multiple sclerosis: results of a phase II clinical trial with an altered peptide ligand. Nat Med. 2000; 6(10): 1167–1175. [DOI] [PubMed] [Google Scholar]
- 47. Thorpy MJ, Krieger AC. Delayed diagnosis of narcolepsy: characterization and impact. Sleep Med. 2014; 15(5): 502–507. [DOI] [PubMed] [Google Scholar]
- 48. Statistik Austria. Impfschutz 2014. http://www.statistik.at/web_de/statistiken/menschen_und_gesellschaft/gesundheit/gesundheitsversorgung/gesundheitsvorsorge/index.html Accessed June 29, 2016.
- 49. Mereckiene J. Seasonal influenza vaccination in Europe—Overview of vaccination recommendations and coverage rates in the EU Member States for the 2012–13 influenza season. Stockholm: European Centre for Disease Prevention and Control. 2015, p. 11. doi:10.2900/693898. [Google Scholar]
- 50. Dauvilliers Y, Jaussent I, Lecendreux M, et al. Cerebrospinal fluid and serum cytokine profiles in narcolepsy with cataplexy: a case-control study. Brain Behav Immun. 2014; 37: 260–266. [DOI] [PubMed] [Google Scholar]
- 51. Lecendreux M, Libri V, Jaussent I, et al. Impact of cytokine in type 1 narcolepsy: role of pandemic H1N1 vaccination ? J Autoimmun. 2015; 60: 20–31. [DOI] [PubMed] [Google Scholar]
- 52. Tanaka S, Honda M, Toyoda H, Kodama T. Increased plasma IL-6, IL-8, TNF-alpha, and G-CSF in Japanese narcolepsy. Hum Immunol. 2014; 75(8): 940–944. [DOI] [PubMed] [Google Scholar]
- 53. Kornum BR, Pizza F, Knudsen S, Plazzi G, Jennum P, Mignot E. Cerebrospinal fluid cytokine levels in type 1 narcolepsy patients very close to onset. Brain Behav Immun. 2015; 49: 54–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.