Abstract
Etiologic factors for pancreatic cancer, the fourth deadliest malignant neoplasm in the United States, include obesity and abnormal glucose metabolism. Calorie restriction (CR) and rapamycin each affect energy metabolism and cell survival pathways via inhibition of mammalian target of rapamycin (mTOR) signaling. Using a Panc02 murine pancreatic cancer cell transplant model in 45 male C57BL/6 mice, we tested the hypothesis that rapamycin mimics the effects of CR on pancreatic tumor growth. A chronic regimen of CR, relative to an ad libitum-fed control diet, produced global metabolic effects such as reduced body weight (20.6±1.6g vs. 29.3±2.3g; p<0.0001), improved glucose responsiveness, and decreased circulating levels of insulin-like growth factor (IGF)-1 (126±8ng/mL vs. 199±11ng/mL; p=0.0006) and leptin (1.14±0.2 ng/mL vs. 5.05±1.2 ng/mL; p=0.01). In contrast, rapamycin treatment (2.5mg/kg i.p. every other day, initiated in mice following 20 weeks of ad libitum control diet consumption), relative to control diet, produced no significant change in body weight, IGF-1 or leptin levels, but decreased glucose responsiveness. Pancreatic tumor volume was significantly reduced in the CR group (221±107mm3; p<0.001) and, to a lesser extent, the rapamycin group (374±206mm3; p=0.04) relative to controls (550±147mm3), and this differential inhibition correlated with expression of the proliferation marker Ki-67. Both CR and rapamycin decreased phosphorylation of mTOR, p70/S6K and S6 ribosomal protein, but only CR decreased phosphorylation of Akt, GSK-3β, ERK/MAPK, and STAT-3TYR705. These findings suggest rapamycin partially mimics the anticancer effects of calorie restriction on tumor growth in a murine model of pancreatic cancer.
Keywords: Pancreatic cancer, Calorie restriction, Rapamycin, Insulin-like growth factor-1, IGF-1, Energy balance, mammalian target of rapamycin, mTOR
Introduction
Effective prevention and treatment strategies are urgently needed for pancreatic cancer, the fourth leading cause of cancer-related death in both males and females in the United States (1). Only 10–15% of pancreatic cancer patients have localized disease amenable to curative resection, and the overall 5-year survival rate in affected patients is <5% (1, 2). Interrelated etiologic factors in pancreatic cancer include obesity, abnormal glucose metabolism, and positive energy balance (defined as caloric intake exceeding energy expenditure) (3–5). Components of energy metabolism pathways thus may be useful targets for pancreatic cancer prevention and control. Calorie restriction (CR) and the drug rapamycin are dietary and pharmacologic interventions, respectively, that act on pathways related to energy metabolism and inhibit various tumor types (6, 7). To our knowledge, the effects of these interventions in pancreatic cancer have not been previously compared.
CR, typically involving a 20–40% reduction in total energy intake but isonutrient for vitamins, minerals, fatty acids, and amino acids relative to an ad libitum-fed control regimen, prevents or reverses obesity, improves insulin sensitivity, and inhibits the development and/or progression of many types of cancer (7). In animal models, the anticancer effects of CR are strongly associated with reductions in circulating levels of the nutrient-responsive mitogen insulin-like growth factor (IGF)-1 (8, 9). For example, CR suppresses the development and pathological severity of murine COX-2-driven pancreatitis and pancreatic cancer through a reduction of circulating IGF-1 levels (10).
Epidemiologic evidence shows that i) pancreatic cancer patients, relative to healthy controls, have higher levels of serum IGF-1 and pancreatic expression of the IGF-1 receptor (IGF-1R), and ii) pancreatic cancer patients with elevated circulating IGF-1, relative to patients with normal levels, have a worse prognosis (11, 12). IGF-1 exerts its effects on cellular growth and metabolism, at least partially through activation of the phosphatidylinositol 3-kinase (PI3K)/ Akt/ mammalian target of rapamycin (mTOR) pathway (13, 14).
Despite the substantial evidence highlighting the beneficial effects of CR, maintaining this lifestyle in humans is extremely challenging (7). This has prompted an intense search for CR mimetics, which are pharmacologic agents that possess anticancer effects similar to CR without restricting energy intake (7). One putative CR mimetic is rapamycin (7). Unlike CR, rapamycin and its analogs affect neither body weight nor energy balance (15). However, rapamycin and CR each suppress signaling through mTOR and extend lifespan in both invertebrates and mammalian species (7, 16–18). The lifespan extension in mammals is primarily due to reduced tumor development (17). mTOR acts as a sensor that integrates growth factor signals, nutrient availability and energy status with translational control of new proteins (19). Pharmacologic inhibition of mTOR by rapamycin halts DNA synthesis and proliferation of pancreatic cancer cells in vitro through regulation of ribosomal S6 kinase and other downstream targets (20, 21). Rapamycin treatment in various xenograft models of pancreatic cancer in immunodeficient mice inhibits tumor burden by impeding cell proliferation and angiogenesis while promoting apoptosis (22, 23). Additionally, recent studies using murine prostatic, lung, and mammary cancer models support a role for rapamycin and its analogs in cancer chemoprevention (24–27).
In the present study, we tested the hypothesis that rapamycin mimics the effects of CR on pancreatic tumor growth using a Panc02 pancreatic tumor cell transplant model. We found that 1) chronic CR decreases pancreatic tumor growth in association with a reduction in prosurvival signaling; 2) rapamycin also reduces tumor growth through targeted inhibition of the mTOR pathway; and 3) rapamycin-induced mTOR inhibition, although effective, does not completely mimic the effects of CR on tumor growth inhibition, metabolism or cell signaling in a pancreatic cancer cell transplant model.
Materials and Methods
Mice
The Institutional Animal Care and Use Committee of the University of Texas approved all mouse experiments. Male C57BL/6 mice were received from Jackson Laboratories (Bar Harbor, ME) between 4–6 weeks of age, singly housed in a semibarrier facility at the University of Texas at Austin Animal Resource Center, and fed a chow diet for a 2-week acclimation period before study initiation.
Interventions
Mice were randomized to receive one of two diets for 30 weeks: a) control diet (Research Diets, Inc., New Brunswick, NJ; #D12450B) consumed ad libitum, n=27; or b) CR diet (Research Diets; #D03020702) consumed in daily aliquots to provide 70% of the energy and 100% of all nutrients (except carbohydrates) relative to the control group, n=18. Food intake and body weights were recorded weekly until Panc02 tumors became palpable (27 weeks of study).
At 16 weeks of study, 5 mice from each diet group were fasted for 12 hours then anesthetized by CO2 inhalation. They then underwent cardiac puncture for blood collection and subsequently were killed by cervical dislocation. After coagulating at room temperature (RT) for 30 minutes, blood samples were centrifuged at 9,300×g for 5 min. Serum was separated, then snap-frozen and stored at −80°C until assayed for hormones. Tissues were collected and flash frozen for subsequent molecular and biochemical studies.
At 20 weeks of study, the remaining mice in the control group (n=22) were randomized to receive (every other day) an intraperitoneal (i.p.) injection of vehicle (0.1% DMSO in 0.9% saline; n=11) or 2.5 mg/kg rapamycin (n=11). The remaining mice in the CR group (n=13) also began receiving vehicle via i.p. injection every other day. This dose was chosen based on reports in the literature showing effective tumor inhibition with rapamycin between 1–10 mg/kg daily or every other day, with the lower doses showing comparable antitumor effects without the toxicity of the higher doses (15, 28). For our study, a moderate dose was selected because of the extended treatment period.
Tumor cell injection and tumor monitoring
Mouse pancreatic cancer cells (Panc02, generously provided by Drs. Ken Hance and Jefferey Schlom, NCI) (29) were cultured under an atmosphere of 5% CO2 in a 37°C incubator with McCoy’s media (HyClone) supplemented with 10% fetal bovine serum (HyClone), penicillin/streptomycin, glutamine, non-essential amino acids, sodium pyruvate, and HEPES. Cells were trypsinized, washed in Hanks’ Buffered Saline Solution (HBSS), centrifuged, and resuspended in HBSS for injection. Karyotyping and species identification of Panc02 cells were verified by the Molecular Cytogenetics Core Facility at The U.T. M.D. Anderson Cancer Center (Houston, TX).
At 22 weeks of study, mice were subcutaneously injected into the right flank with 1×106 Panc02 cells. One mouse from the control and CR groups each and two mice from the control plus rapamycin group died before tumor development within two weeks of Panc02 injection, and were thus censored from subsequent analyses. Once palpable, tumors were measured with calipers weekly until approximately half of tumors from any group were ≥ 1.5 cm in diameter. Tumor volume was approximated using the formula for an ellipsoid (4/3π(r1)2(r2)). At study termination, all remaining mice were fasted for 12 hours then anesthetized by CO2 inhalation. They then underwent cardiac puncture for blood collection and subsequently were killed by cervical dislocation. Blood samples were processed as detailed above. Pancreatic tumors were harvested and either snap-frozen in liquid nitrogen and stored at −80°C, or fixed with 10% neutral buffered formalin overnight and then switched to 70% ethanol, paraffin embedded, and used for histologic and immunohistochemical analyses as described below.
Glucose Tolerance Test (GTT)
A GTT was performed, as previously described (30), on randomly selected mice from the control and CR groups at 14 weeks of study (n=12 per group). At 22 weeks of study, following two weeks of rapamycin or vehicle treatment and before Panc02 cell injection, a second GTT was performed on a subset of 10 mice from each diet/drug group.
Energy balance-related serum hormones
Serum IGF-1 was measured using radioimmunoassay according to manufacturer’s instructions (DSL-2900 kit, DSL/Beckman Coulter Laboratories, Webster, TX). Serum insulin and leptin were measured using Lincoplex® bead-based assays (Millipore Corporation, Billerica, MA) on a BioRad Bioplex® analyzer (BioRad, Hercules, CA) according to manufacturer’s directions. Analyses were conducted on samples obtained at 16 weeks, before Panc02 cell injection (to assess diet-induced changes in the absence of potentially confounding tumor effects on circulating hormone levels; n=5 per group) and at study termination (to exclude the possibility that rapamycin affected circulating levels within the control group; control, n=6; rapamycin-treated control, n=3).
Histopathology and immunohistochemistry
Formalin-fixed pancreatic tumors were embedded in paraffin and then cut into 4-µm thick sections and processed for either hematoxylin and eosin (H&E) or immunhistochemical staining at the Histology Core Laboratory at The U.T. M.D. Anderson Cancer Center, Science Park Research Division (Smithville, TX). Antibodies used for immunohistochemistry were optimized by core personnel using both positive and negative controls that were repeated with each analysis. Slides were deparaffinized and hydrated sequentially in ethanol and water. Antigen retrieval required microwaving slides for 10 min with 10mM citrate buffer. Endogenous peroxidase activity was quenched with 3% hydrogen peroxide for 10 min.
Nonspecific binding was blocked with Biocare blocking reagent (Biocare Medical, Concord, CA) for 30 min at RT, then sections were incubated with primary antibody diluted in blocking buffer. The following primary antibodies (source, dilution and incubation conditions presented parenthetically) were used: Ki-67 (Dako, Carpenteria, CA; 1:200, 4°C overnight); phospho-IGF1R Tyr1131 and IGF1R (Cell Signaling, Danvers, MA; 1:50, 4°C overnight); phospho-AktSer473 (Santa Cruz Biotechnology, Santa Cruz, CA; 1:50, 1 h RT); Akt (Cell Signaling; 1:100; 4°C overnight) phospho-GSK-3βSer9 (Santa Cruz Biotechnology; 1:50, 1 h RT); GSK-3β (Millipore; 1:200; 1 h RT); phospho-ERKThr202/Tyr204 (Cell Signaling; 1:100; 1 h RT); ERK (Cell Signaling; 1:25; 1 h RT); phospho-Stat3Tyr705 (Cell Signaling; 1:50; 4°C overnight); phospho-Stat3Ser727 (Cell Signaling; 1:50, 4°C overnight); STAT3 (Cell Signaling; 1:100; 1 h RT); phospho-mTORSer2448 (Cell Signaling; 1:50, 4°C overnight); mTOR (Cell Signaling; 1:100; 1 h RT); phospho-S6 ribosomal protein(Ser235/236) (Cell Signaling; 1:50, 1 h RT); S6 (Cell Signaling; 1:100; 4°C overnight) and cyclin D1 (Santa Cruz Biotechnology; 1:500, 2h RT). Slides were washed twice in PBS, incubated with horseradish peroxidase (HRP)-labeled α-rabbit secondary antibody (Dako) for 30 minutes at RT at a concentration of 1:200 with the following exceptions: a) Ki-67 (rabbit anti-rat IgG; 1:200, 30 min RT; Vector, Burlingame, CA); b) phospho-STAT3 and phospho-mTOR (rabbit HRP-polymer; 30 min RT; Biocare, Concord, CA); and c) cyclin D1 (rabbit anti-mouse F(ab)’; 1:250, 15 min RT; Accurate Chemical, Westbury, NY). Slides were then washed five times with PBS. Diaminobenzidine was used to develop the antibody staining followed with a hematoxylin counterstain. Images were captured using a light microscope equipped with a digital camera (Leica Camera Inc, Allendale, NJ). Immunohistochemically-stained tumor sections were assigned a score based on the following criteria: 1=mild (majority of tumor section exhibited weakly positive staining pattern or <50% of cells in field stained an equivalent intensity to control tumors), 2=moderate (majority of tumor section exhibited moderate-to-dark brown stain or 50–75% of cells in field stained an equivalent intensity to control tumors), or 3=marked (majority of tumor section exhibited dark brown stain or >75% of cells in field stained an equivalent intensity to control tumors). The quality of staining determined whether the intensity of stain or percentage of stained cells in field was quantified. For example, the antibodies against phospho-IGF1-R and phospho-ERK produced weak but consistent signal intensity; therefore, the percentage of stained cells in field was assessed. Sample size was determined based on quality of tissue fixation/staining. More tumors were used for analysis using the phosphorylated IGF1R, Akt, GSK-3β, ERK, STAT3, mTOR, and S6 ribosomal protein antibodies, and total cyclin D1 antibody (for each antibody: control, n=4; rapamycin-treated control, n=7; CR, n=5) than Ki-67 (n=3/group) because the latter yielded a more easily quantifiable nuclear staining pattern. Images were captured at 40X magnification (with the exception of cyclin D1 which was captured at 20X) in 3–4 fields in a tumor section from each tumor analyzed.
Western blotting
Pancreatic tumors were homogenized and lysed in RIPA buffer (Sigma, St. Louis, MO) with protease inhibitor tablet (Roche Applied Sciences, Indianapolis, IN) and phosphatase inhibitor cocktails I and II (Sigma). Protein lysates (50–80µg) were resolved by SDS-PAGE using 6, 10, or 12% gels, transferred to PVDF membranes (Bio-Rad, Hercules, CA), and blocked using LI-COR Blocking Buffer (LI-COR Biotechnologies, Lincoln, NE). Membranes were incubated overnight at 4°C with primary antibody (from Cell Signaling unless otherwise stated) diluted in blocking buffer and specific for: phospho-AktSER473 (1:500); Akt (1:1000); actin (1:1000); phospho-GSK-3βSer9(Santa Cruz, 1:1000); GSK-3β (Millipore, 1:1000); phospho-ERKThr202/Tyr204(1:1000); ERK (1:1000); phospho-mTORSer2448(1:500); mTOR (1:1000); phospho-p70/S6KThr389 (1:500); p70/S6K (1:1000); and myosin IIa (1:1000). Actin was used as a loading control for all antibodies except mTOR (for which myosin IIa was used because the 6% polyacrylamide gel used to resolve mTOR did not retain actin). After 3 washes (5 min each) in 0.1% Tween-20/PBS (PBS-T), membranes were incubated for 1 h at RT in species-specific secondary antibody (LI-COR Biotechnologies) diluted in LI-COR blocking buffer (1:5000). Following three washes in PBS-T, membranes were scanned using the Odyssey infrared fluorescent imaging system. Densitometry was performed using LI-COR software (LI-COR Biotechnologies). Relative expression of phosphorylated proteins was calculated using 3 tumors per group.
Statistical analyses
Data are presented as mean ± standard deviation, except serum hormone levels and Ki-67 which are presented as mean ± standard error of the mean. Statistical analyses were conducted using SPSS (Apache Software Foundation, Wilmington, DE). Temporal differences between groups with respect to body weight and caloric intake were assessed using repeated measures analysis; final measurements were compared using independent t-tests. Pretumor serum hormone levels between the control and CR groups were compared using independent t-tests. Pair-wise comparisons of glucose tolerance and tumor burden as a function of time and treatment group were performed using a linear mixed-effects model. Final tumor volume measurements were compared using independent t-tests. Differences between groups in immunohistochemical staining of 1) Ki-67 were determined by one-way ANOVA followed by Tukey’s post-hoc test of significance and 2) all other antibodies were determined by Fisher exact test. Differences in western blot densitometry between each test group (rapamycin-treated controls and CR), relative to the control group, were compared by independent t-tests. Results were considered significant if p <0.05.
Results
Effects of CR on body weight, glucose tolerance, and serum hormone levels
Male C57BL/6 mice were fed either a control diet known to result in an overweight phenotype or a 30% CR diet (7) for 30 weeks (including 22 weeks of diet before Panc02 cell injection). Relative to controls, the CR mice had significantly reduced body weights beginning as early as 3 weeks on study (p<0.01) (Fig. 1A–B). Diet-dependent effects on body weight continued throughout the study and, at 27 weeks, mean body weights were 20.6±1.6 g in CR mice (n=12; p<0.0001) and 29.3±2.3 g in controls (n=10).
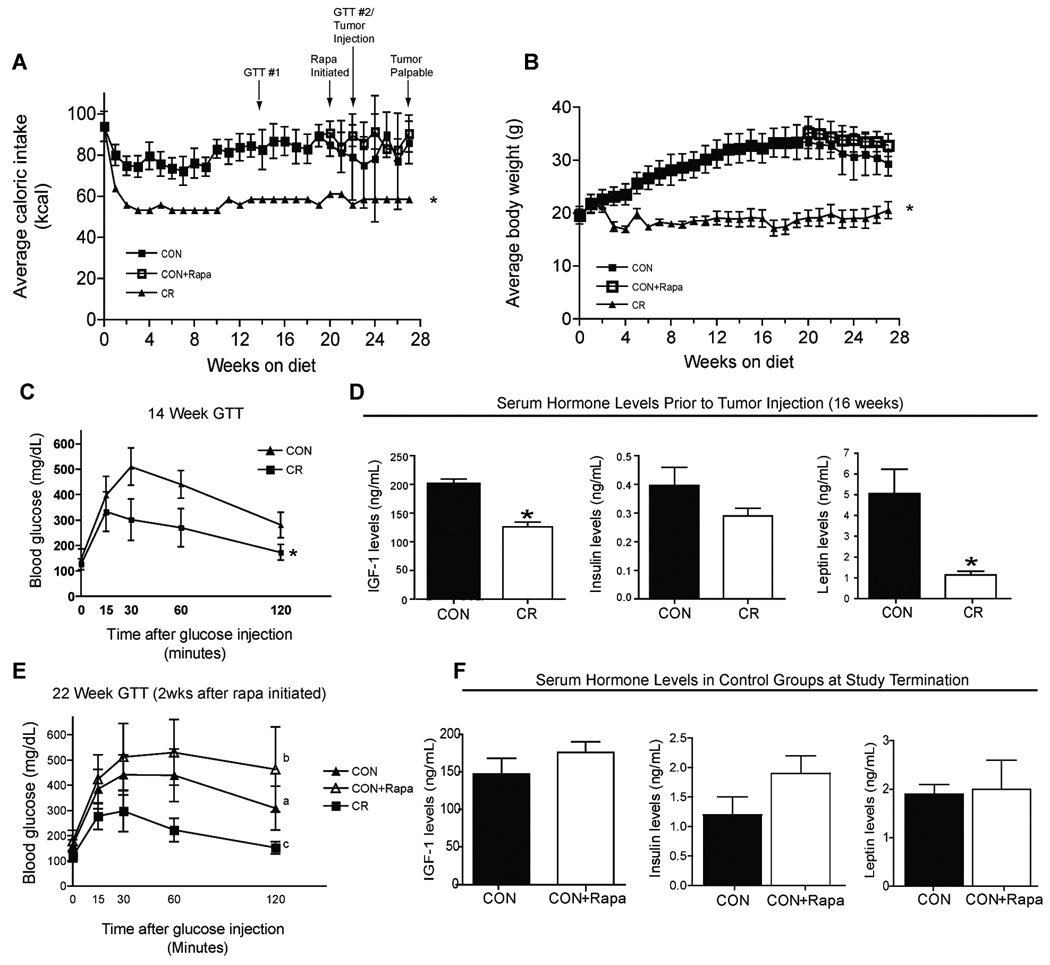
Figure 1. Effects of calorie restriction versus rapamycin on food intake, body weight, glucose tolerance, and serum hormone levels.
A,B, C57BL/6 male mice fed a CR diet (n=12) for 27 weeks consumed fewer calories and weighed significantly less than mice fed a control diet (CON; n=10). Within the mice receiving control diet, a 10 week rapamycin treatment (CON+Rapa; n=9), initiated at 20 weeks of study, had no significant effect on caloric intake or body weight relative to the control mice administered vehicle (n=10). C, GTT performed on a subset of mice fed either a control or CR diet for 14 weeks (n=12/group). D, Pretumor serum levels of IGF-1, insulin, and leptin in a subset of mice fed either a control or CR diet for 16 weeks (n=5/group). E, GTT performed at 22 weeks of study (immediately prior to Panc02 cell injection) on mice fed CR or control diet and administered vehicle or rapamycin beginning at week 20 of the study (n=10/group). F, Posttumor serum levels (at study termination) of IGF-1, insulin and leptin in mice receiving the control diet + vehicle (CON, n=6) versus the control diet + rapamycin (CON+Rapa n=3). A–C & E, error bars represent SD. D&E, error bars represent SEM. A–D, significant differences (p<0.05) are denoted with *. E, different letters denote significant differences; F, no values were significantly different.
The CR group, relative to control, displayed enhanced glucose tolerance as assessed by GTT. At 14 weeks of study (Fig. 1C), blood glucose concentrations following glucose bolus injection in CR mice peaked at 15 minutes and averaged 332±78 mg/dL, while the control group peaked at 30 minutes and averaged 510±73 mg/dL (n=12 per group). After the peaks were achieved, blood glucose concentrations remained consistently lower in the CR mice (p<0.0001 for between-group comparison at the 120-minute measurement). Comparable diet-dependent effects on glucose tolerance were noted at 22 weeks of study, at which time the CR and control mice had been receiving, for 2 weeks, vehicle by i.p. injection every other day (Fig. 1E; n=10 each).
In a subset of mice fed for 16 weeks and then bled (n=5 per group), the CR mice had significantly lower serum levels of IGF-1 (126±8 ng/mL; p=0.0006) and leptin (1.14±0.17 ng/mL; p=0.01) than control mice (199±11 ng/mL and 5.05±1.18 ng/mL, respectively; Fig. 1D). No between-group difference in serum insulin levels was detected (p=0.15).
Effects of rapamycin on body weight, glucose tolerance, and serum hormones
Beginning at 20 weeks of study, the control mice received their assigned diet plus i.p. injections every other day of either 2.5 mg/kg rapamycin (for the control diet plus rapamycin group, n=9) or vehicle (control, n=10). The CR group (n=12) also received vehicle. Moderate reduction of caloric intake in the control group was noted between weeks 22 and 24 relative to the control plus rapamycin group (Fig. 1A). However, this decrease did not approach statistical significance, nor did it significantly affect body weight (Fig. 1B). This modest differential between the two groups subsided by week 25. Between weeks 20–27 of study, body weights remained stable within each diet/drug group and at 27 weeks were comparable between the control mice (29.3±2.3 g) and rapamycin-treated mice (32.8±2.1 g; Fig. 1A). As previously mentioned, the CR mice were leaner than the others.
The average peak glucose levels in the rapamycin-treated mice (530±130 mg/dL) occurred 60 minutes after the glucose bolus was administered whereas control mice receiving vehicle peaked at 30 minutes and only reached, on average, 441±80 mg/dL (Fig. 1E). Moreover, blood glucose levels at the final time point (120 minutes after glucose bolus) were significantly higher in rapamycin-treated mice (462±169 mg/dL; p=0.02) relative to the control plus vehicle group (309±87 mg/dL). Consistent with the GTT results at 14 weeks, CR mice, as compared with the others, exhibited the lowest levels of glucose at all points including the final assessment (151±24 mg/dL; p<0.0001).
To exclude the possibility that rapamycin impacts circulating energy balance-related hormones relative to the control plus vehicle group, serum collected at study termination was assessed for levels of IGF-1, insulin, and leptin (Fig 1F). No statistical differences (all p>0.15) were detected between rapamycin-treated mice (n=3) and controls (n=6), respectively, in circulating levels of IGF-1 (176±14 vs. 147±21 ng/mL), insulin (1.9±0.3 vs. 1.2±0.3 ng/mL), or leptin (2.0±0.6 vs. 1.9±0.2 ng/mL).
Effects of CR and rapamycin on Panc02 tumor growth and histology
To compare the anticancer effects of CR and rapamycin interventions, we injected mice from each diet/drug group with Panc02 cells at week 22 and monitored tumor growth during the next 8 weeks. Tumors in rapamycin-treated mice (p=0.009) and CR mice (p<0.0001) grew significantly slower than in control mice receiving vehicle. CR exerted a more dramatic inhibitory effect than rapamycin as evidenced by a significant difference between their tumor growth (p=0.005; Fig. 2A). Final tumor volumes from rapamycin-treated mice (374±206 mm3; p=0.04) and CR mice (221±107 mm3; p<0.0001) were significantly smaller on average than controls (550±147 mm3). The CR and rapamycin interventions each delayed tumor onset, with only 17% and 33% of mice, respectively, having palpable tumors 6 weeks after Panc02 cell injection compared to 89% of the control group (Fig. 2B). Only at study termination did all mice in the CR and control diet plus rapamycin groups have detectable tumors.
Figure 2. Effect of calorie restriction versus rapamycin treatment on tumor growth and histology.
A, weekly tumor measurements were taken using calipers beginning when the first tumor became palapable (5 weeks) after Panc02 cells were subcutaneously injected into C57BL/6 mice receiving the control diet plus vehicle (CON, n=10), control diet plus rapamycin (CON + Rapa, n=9), or CR diet plus vehicle (n=12). Error bars represent SD. B, Percentage of mice in each diet/drug group with palpable tumor at weeks 5, 6, 7 and 8 after Panc02 cell injection. C, Immunohistochemical staining for Ki-67 expression and H&E staining of tumors. Scale bars for Ki-67, 100µm and H&E, 400µm. Arrows indicate adipocytes. D, Quantification of Ki-67-positive cells from representative images captured at 40X magnification. Data are expressed as mean ± SEM number of Ki-67-positive cells/field in tumors (n=3). Values with different letters are significantly different at p < 0.05.
The influence of CR or rapamycin treatment on cell proliferation was assessed in tumor tissues by immunohistochemical staining against Ki-67 (Fig. 2C and D). CR (74.8±9.9 positive cells/field; n=3; p=0.001) and rapamycin treatment (141.9±11.0 positive cells/field; n=3; p=0.013) each significantly reduced cell proliferation (based on Ki-67 immunopositivity) relative to controls (231.7±21.3 positive cells/field; n=3). CR produced a more substantial reduction in proliferation (p=0.04) relative to rapamycin treatment.
The effect of CR and rapamycin intervention on tumor histology was qualitatively assessed using H&E staining (Fig. 2C). There was a considerable presence of adipocytes in the control tumors that was not seen in the CR tumors. Unlike CR, rapamycin treatment did not lessen the level of adipocyte infiltration associated with the control diet.
Effects of CR and rapamycin on signaling intermediates
Based on immunohistochemical analysis of signaling intermediates, CR tumors relative to control tumors displayed reduced expression of phosphorylated Akt (p=0.03), ERK (p=0.05), STAT-3Tyr705 (p=0.02), STAT-3Ser727 (p=0.01), mTOR (p=0.02), S6 ribosomal protein (p=0.004), GSK-3β (p=0.06), IGF1-R (p=0.11), and cyclin D1 (p=0.11) (Fig. 3A–B). Rapamycin produced a more selective signaling profile than CR in which only pSTAT-3Ser727 (p=0.02) and mTOR pathway components were inhibited relative to control, including phospho-mTOR (p=0.02), phospho-S6 ribosomal protein (p=0.006) (Fig. 3A–B), but not phospho-IGF-1R (p=1), phospho-Akt (p=0.3), phospho-GSK-3β (p=1), phospho-ERK (p=0.54), or phospho-STAT3TYR705 (p=0.24). No appreciable changes to total protein expression were noted (data not shown).
Figure 3. Effect of CR and rapamycin on signaling pathways in pancreatic tumors by immunohistochemical analysis.
A, Immunhistochemical analyses of phosphorylated IGF1R, Akt, GSK-3β, ERK, STAT3, mTOR, and S6 ribosomal protein as well as total protein expression of cyclin D1. Scale bars, 100µm except cyclin D1, 200µm. B, Quanitification of antibody staining patterns. Tumors were assigned a score that represented the majority of the section: 1 (mild-white), 2 (moderate-gray), or 3 (maximal-black). The bar graph represents the percentage of tumors in that group associated with the corresponding score assignment (CON, n=4; CON+rapa, n=7; CR, n=5). Values with different letters are significantly different at p < 0.05.
Immunoblotting of various signaling intermediates confirmed the dampening of other survival signals in CR tumors (Fig. 4A). CR (n=3) significantly reduced phosphorylation of Akt (p=0.006), GSK-3β (p=0.04), ERK (p=0.004), mTOR (p=0.05), and p70/S6K (p=0.05) relative to the control diet which, despite an occasionally variable expression pattern, had higher levels of phosphorylated proteins when averaged over three tumors (Fig. 4B). Rapamycin potently and consistently reduced phosphorylation of mTOR (p=0.005) and p70/S6K (p=0.02) when compared to control tumors, and decreased phosphorylation of p70/S6K more robustly than did CR (p=0.008) (Fig. 4B). Despite the potent inhibitory effects of rapamycin on mTOR signaling intermediates, levels of phosphorylated Akt, GSK-3β and ERK were similar to control tumors (Fig. 4A). Neither CR nor rapamycin had a significant effect on total protein expression of Akt, mTOR, p70/S6K, GSK3b, or ERK (Fig. 4A).
Figure 4. Effect of CR and rapamycin on signaling pathways in pancreatic tumors by immunoblot analysis.
A, Immunoblotting analyses of phosphorylated and total protein expression of Akt, GSK-3β, ERK, mTOR, and p70/S6K. Data shown are representative blots from at least 3 tumors for each treatment. B, Relative phosphorylation of phospho-Akt, phospho-GSK3b, phospho-ERK, phospho-mTOR, and phospho-p70/S6K proteins, quantified by densitometry using LI-COR Odyssey software. Data represent mean of 3 tumors/group; error bars represent SD. Significance denoted by * or different letters (p<0.05).
Discussion
CR is effective at inhibiting cancer growth in many model systems (7). Although we found a strong anticancer effect of CR in a COX-2-driven transgenic model of pancreatic neoplasia (10), we sought to establish and understand the growth prohibitive effects of CR on transplanted pancreatic tumors. In addition, we wanted to compare the anticancer effects of a chronic CR dietary regimen versus an acute pharmacological intervention, rapamycin, which share several downstream signaling targets but have not been directly compared in a pancreatic cancer model. We found in C57BL/6 mice that CR (relative to a control diet fed ad libitum that results in overweight mice) reduced Panc02 tumor burden. Furthermore, we established that exposure to rapamycin (at a dose of 2.5 mg/kg ip every other day, which effectively inhibited mTOR without toxicity) also significantly suppressed Panc02 tumor growth, although to a lesser extent than CR. Central to both interventions is an ability to dampen signaling through the mTOR pathway, a highly conserved protein at the crux of intracellular energy sensing and external growth factor signaling. However, the unique ability of CR to alter multiple signaling pathways involved in proliferation and survival was more influential on pancreatic tumor growth than the selective targeting of mTOR with rapamycin.
Our finding that chronic CR (30 weeks), relative to control diet, inhibited Panc02 tumor growth in association with improved insulin sensitivity and reduced circulating IGF-1 and leptin, is consistent with established links between altered metabolism and pancreatic cancer. Specifically, there is a two-fold higher risk for developing pancreatic cancer in the context of altered glucose metabolism, such as that occurring in diabetes (4, 31). Although fasting levels of insulin were moderately but not statistically decreased in the CR group (p=0.08), the functional sensitivity of CR mice to insulin was dramatically improved relative to the control group, as indicated by GTT. The antidiabetic biguanide metformin improves insulin resistance, reduces pancreatic cancer risk in type II diabetics by 62% (32), and also prevents development of carcinogen-induced pancreatic lesions enhanced by a high-fat diet in hamsters (33), suggesting improved glucose metabolism and/or mTOR inhibition may contribute to decreased pancreatic cancer development.
In addition to improved responsiveness to insulin in the CR group, there was a significant decrease in serum levels of IGF-1. This is important given the connection between pancreatic cancer risk and serum levels of IGF-1 in human subjects (11, 12), and the implication that reduced IGF-1 underlies many of the anticancer effects of CR (8, 10). The protective effects of reduced IGF-1 signaling in a skin carcinogenesis model have been associated with an abrogation in mTOR signaling (9). The current study recapitulates this connection between CR, reduced circulating IGF-1, and subsequently diminished Akt/mTOR signaling. It also shows that CR dampened other components of prosurvival signaling such as GSK-3β, ERK, and STAT3. While this is not a comprehensive assessment of proliferation and survival signaling pathways, these findings suggest that the ability to suppress multiple pathways underlies the potent and broad-acting anticancer effects of CR.
Our studies also aimed to establish and understand the pancreatic cancer therapeutic potential of rapamycin. Recently, several reports have offered evidence that mTOR inhibitors might have cancer preventive activity, at least in part by mimicking some effects of CR (24–27). For example, low-dose rapamycin treatment of HER-2/neu mice significantly diminished tumor formation, with one third of mice having no detectable tumors at sacrifice (26). In a mouse prostate model expressing human AKT1, the rapamycin analog, RAD001, reversed prostatic intraepithelial neoplasia by enhancing apoptosis and abrogating expression of HIF-1α genes (25). Another rapamycin analog, CCI-779, abrogates progression of lung adenomas that are induced by activating K-RAS mutations (25–27, 34). Sensitivity to mTOR inhibition is enhanced in tumors that rely on PI3K/Akt signaling such as those with a deficiency in the phosphatase and tensin homolog (PTEN) tumor suppressor (35–37). Excessive activation of the PI3K/AKT pathway may be largely responsible for the detrimental effects of obesity (38). Thus, it seems plausible that rapamycin treatment could overcome the growth-promoting effects of excessive energy intake.
Our findings show that treatment with rapamycin circumvents some of the protumorigenic effects of the calorie-dense control diet. This effect is seen in our rapamycin-treated mice despite insulin resistance, elevated serum levels of IGF-1 and leptin, and other metabolic parameters typically associated with enhanced tumor growth. Rapamycin treatment actually resulted in a worsened sensitivity to a glucose bolus than the control group, despite having no effect on caloric intake and body weights. The alteration in glucose homeostasis in response to rapamycin is consistent with findings in the P. obesus diabetic rat model in which insulin resistance is enhanced by rapamycin because of increased β cell apoptosis, decreased β cell mass, and reduced glucose-induced insulin biosynthesis and secretion from islet cells (39). Moreover, chronic rapamycin treatment stimulates hepatic gluconeogenesis (40), which could further disrupt glucose homeostasis. These metabolic outcomes of mTOR inhibition potentially enhance glucose bioavailability to cancer cells, possibly offsetting some of the growth-inhibitory effects of rapamycin. Despite these metabolic alterations, including high levels of circulating mitogens, mTOR signaling was substantially inhibited by rapamycin (even to a greater extent than by CR), resulting in pancreatic tumor growth suppression. This further supports the mTOR pathway as an important target for pancreatic cancer prevention and control.
In addition to disparate responses to insulin and glucose between the CR and rapamycin interventions, signaling patterns were also divergent. Although both interventions diminished mTOR signaling, rapamycin did not inhibit other survival signals such as ERK, GSK-3β, and STAT3TYR705. Akt phosphorylation in the tumors from the rapamycin-treated group was generally higher than in tumors from the control group. This is consistent with a known diminution of an S6K-mediated feedback inhibition that can result in Akt activation in response to mTOR inhibitors (41–44). However, rapamycin reduced phosphorylation of an mTOR-sensitive residue (Serine 727) on pSTAT3 that is necessary for full transcriptional activation of STAT3 (45). It is plausible that the transcriptional activity of STAT3 (which we did not assess in our system), is dampened by rapamycin when compared to control tumors, but not CR tumors, especially considering CR resulted in reduced phosphorylation at both the TYR705 and SER727 sites.
A histological difference between tumors from CR and rapamycin-treated mice was also noted. Adipocytes were consistently present in the tumors from mice receiving the control diet, regardless of whether they received rapamycin or vehicle. In contrast, CR clearly reduced adipocyte infiltration into tumors. Zhang et al. (2009) showed that stromal and endothelial cells from adipose tissue migrate to tumors and promote tumor growth, and that endogenous white adipose tissue (enhanced in an overweight or obese state) was the source of the adipose progenitors infiltrating the tumors (46). Furthermore, studies show that coadministration of tumor cells with mouse adipose cells promote tumor take and growth (47, 48). Further contributing to potential growth-promoting effects of local adipocytes is the release of soluble adipokines/cytokines (49), one of which (leptin) was elevated in the serum of mice in our study receiving the high-calorie control diet, irrespective of treatment with rapamycin or vehicle. As recently suggested by Subbaramaiah et al., multiple energy balance-related signals contribute to inflammatory crosstalk between macrophages, adipocytes, and epithelial tumor cells (50, 51).
Taken together, our findings show that CR had a stronger inhibitory effect on Panc02 tumor growth than did rapamycin. CR and rapamycin decreased phosphorylation of mTOR pathway components, but only CR reduced circulating IGF-1 and leptin levels and phosphorylation of Akt, GSK-3β, ERK/MAPK, and STAT-3βTYR705. Thus treatment with rapamycin, which specifically inhibited mTOR and significantly decreased Panc02 tumor growth relative to control diet, only partially mimics (at the dose used) the more potent effects of CR on multiple pro-growth signals and pancreatic tumor growth inhibition. This observation that CR, relative to rapamycin, is a more potent suppressor of pancreatic tumor growth and is more promiscuous in terms of targeting multiple signaling pathways suggests that combination approaches (such as an mTOR inhibitor plus a lifestyle or pharmacologic intervention that targets other key pathways) will be most effective for the prevention and control of pancreatic cancer. Future studies are being designed to verify the hypothesis that a synergistic effect is exerted on tumor inhibition when the broader-acting effects of CR are combined with low-to-intermediate doses of pharmacologic mTOR inhibitors such as rapamycin.
Acknowledgements
The authors thank Drs. John DiGiovanni and Phil Dennis for assistance with rapamycin dose selection, Drs. Ken Hance and Jeff Schlom for generously providing the Panc02 cells, and Dr. Donna Kusewitt for assistance with quantification of immunohistochemical staining patterns.
Grant Support: R01 CA135386 (S Hursting and S Fischer); R25T CA57730 and T32 CA135386 (L Lashinger).
Footnotes
No potential conflicts of interest.
References
- 1.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA: a cancer journal for clinicians. 2009 Jul–Aug;59(4):225–249. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.Lillemoe KD, Yeo CJ, Cameron JL. Pancreatic cancer: state-of-the-art care. CA: a cancer journal for clinicians. 2000 Jul–Aug;50(4):241–268. doi: 10.3322/canjclin.50.4.241. [DOI] [PubMed] [Google Scholar]
- 3.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. The New England journal of medicine. 2003 Apr 24;348(17):1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 4.Gapstur SM, Gann PH, Lowe W, Liu K, Colangelo L, Dyer A. Abnormal glucose metabolism and pancreatic cancer mortality. Jama. 2000 May 17;283(19):2552–2558. doi: 10.1001/jama.283.19.2552. [DOI] [PubMed] [Google Scholar]
- 5.Silverman DT, Swanson CA, Gridley G, Wacholder S, Greenberg RS, Brown LM, et al. Dietary and nutritional factors and pancreatic cancer: a case-control study based on direct interviews. Journal of the National Cancer Institute. 1998 Nov 18;90(22):1710–1719. doi: 10.1093/jnci/90.22.1710. [DOI] [PubMed] [Google Scholar]
- 6.Bjornsti MA, Houghton PJ. The TOR pathway: a target for cancer therapy. Nat Rev Cancer. 2004 May;4(5):335–348. doi: 10.1038/nrc1362. [DOI] [PubMed] [Google Scholar]
- 7.Hursting SD, Smith SM, Lashinger LM, Harvey AE, Perkins SN. Calories and carcinogenesis: lessons learned from 30 years of calorie restriction research. Carcinogenesis. 2010 Jan;31(1):83–89. doi: 10.1093/carcin/bgp280. [DOI] [PubMed] [Google Scholar]
- 8.Dunn SE, Kari FW, French J, Leininger JR, Travlos G, Wilson R, et al. Dietary restriction reduces insulin-like growth factor I levels, which modulates apoptosis, cell proliferation, and tumor progression in p53-deficient mice. Cancer research. 1997 Nov 1;57(21):4667–4672. [PubMed] [Google Scholar]
- 9.Moore T, Carbajal S, Beltran L, Perkins SN, Yakar S, Leroith D, et al. Reduced susceptibility to two-stage skin carcinogenesis in mice with low circulating insulin-like growth factor I levels. Cancer research. 2008 May 15;68(10):3680–3688. doi: 10.1158/0008-5472.CAN-07-6271. [DOI] [PubMed] [Google Scholar]
- 10.Lashinger LM, Malone LM, McArthur MJ, Goldberg JA, Daniels EA, Pavone A, et al. Genetic Reduction of Insulin-like Growth Factor-1 Mimics the Anticancer Effects of Calorie Restriction on Cyclooxygenase-2-Driven Pancreatic Neoplasia. Cancer Prev Res (Phila) 2011;4 doi: 10.1158/1940-6207.CAPR-11-0027. XXX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karna E, Surazynski A, Orlowski K, Laszkiewicz J, Puchalski Z, Nawrat P, et al. Serum and tissue level of insulin-like growth factor-I (IGF-I) and IGF-I binding proteins as an index of pancreatitis and pancreatic cancer. International journal of experimental pathology. 2002 Oct;83(5):239–245. doi: 10.1046/j.1365-2613.2002.00237.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lin Y, Tamakoshi A, Kikuchi S, Yagyu K, Obata Y, Ishibashi T, et al. Serum insulin-like growth factor-I, insulin-like growth factor binding protein-3, and the risk of pancreatic cancer death. International journal of cancer. 2004 Jul 1;110(4):584–588. doi: 10.1002/ijc.20147. [DOI] [PubMed] [Google Scholar]
- 13.Taniguchi CM, Emanuelli B, Kahn CR. Critical nodes in signalling pathways: insights into insulin action. Nature reviews. 2006 Feb;7(2):85–96. doi: 10.1038/nrm1837. [DOI] [PubMed] [Google Scholar]
- 14.Pollak M. Insulin and insulin-like growth factor signalling in neoplasia. Nat Rev Cancer. 2008 Dec;8(12):915–928. doi: 10.1038/nrc2536. [DOI] [PubMed] [Google Scholar]
- 15.Wu Q, Kiguchi K, Kawamoto T, Ajiki T, Traag J, Carbajal S, et al. Therapeutic effect of rapamycin on gallbladder cancer in a transgenic mouse model. Cancer research. 2007 Apr 15;67(8):3794–3800. doi: 10.1158/0008-5472.CAN-06-3214. [DOI] [PubMed] [Google Scholar]
- 16.Kapahi P, Zid BM, Harper T, Koslover D, Sapin V, Benzer S. Regulation of lifespan in Drosophila by modulation of genes in the TOR signaling pathway. Curr Biol. 2004 May 25;14(10):885–890. doi: 10.1016/j.cub.2004.03.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harrison DE, Strong R, Sharp ZD, Nelson JF, Astle CM, Flurkey K, et al. Rapamycin fed late in life extends lifespan in genetically heterogeneous mice. Nature. 2009 Jul 16;460(7253):392–395. doi: 10.1038/nature08221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vellai T, Takacs-Vellai K, Zhang Y, Kovacs AL, Orosz L, Muller F. Genetics: influence of TOR kinase on lifespan in C. elegans. Nature. 2003 Dec 11;426(6967):620. doi: 10.1038/426620a. [DOI] [PubMed] [Google Scholar]
- 19.Petroulakis E, Mamane Y, Le Bacquer O, Shahbazian D, Sonenberg N. mTOR signaling: implications for cancer and anticancer therapy. British journal of cancer. 2006 Jan 30;94(2):195–199. doi: 10.1038/sj.bjc.6602902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shah SA, Potter MW, Ricciardi R, Perugini RA, Callery MP. FRAP-p70s6K signaling is required for pancreatic cancer cell proliferation. The Journal of surgical research. 2001 May 15;97(2):123–130. doi: 10.1006/jsre.2001.6145. [DOI] [PubMed] [Google Scholar]
- 21.Grewe M, Gansauge F, Schmid RM, Adler G, Seufferlein T. Regulation of cell growth and cyclin D1 expression by the constitutively active FRAPp-70s6K pathway in human pancreatic cancer cells. Cancer research. 1999 Aug 1;59(15):3581–3587. [PubMed] [Google Scholar]
- 22.Stephan S, Datta K, Wang E, Li J, Brekken RA, Parangi S, Thorpe PE, et al. Effect of rapamycin alone and in combination with antiangiogenesis therapy in an orthotopic model of human pancreatic cancer. Clin Cancer Res. 2004 Oct 15;10(20):6993–7000. doi: 10.1158/1078-0432.CCR-04-0808. [DOI] [PubMed] [Google Scholar]
- 23.Wang Y, Zhao Q, Ma S, Yang F, Gong Y, Ke C. Sirolimus inhibits human pancreatic carcinoma cell proliferation by a mechanism linked to the targeting of mTOR/HIF-1 alpha/VEGF signaling. IUBMB life. 2007 Nov;59(11):717–721. doi: 10.1080/15216540701646484. [DOI] [PubMed] [Google Scholar]
- 24.Namba R, Young LJ, Abbey CK, Kim L, Damonte P, Borowsky AD, et al. Rapamycin inhibits growth of premalignant and malignant mammary lesions in a mouse model of ductal carcinoma in situ. Clin Cancer Res. 2006 Apr 15;12(8):2613–2621. doi: 10.1158/1078-0432.CCR-05-2170. [DOI] [PubMed] [Google Scholar]
- 25.Majumder PK, Febbo PG, Bikoff R, Berger R, Xue Q, McMahon LM, et al. mTOR inhibition reverses Akt-dependent prostate intraepithelial neoplasia through regulation of apoptotic and HIF-1-dependent pathways. Nat Med. 2004 Jun;10(6):594–601. doi: 10.1038/nm1052. [DOI] [PubMed] [Google Scholar]
- 26.Liu M, Howes A, Lesperance J, Stallcup WB, Hauser CA, Kadoya K, et al. Antitumor activity of rapamycin in a transgenic mouse model of ErbB2-dependent human breast cancer. Cancer research. 2005 Jun 15;65(12):5325–5336. doi: 10.1158/0008-5472.CAN-04-4589. [DOI] [PubMed] [Google Scholar]
- 27.Wislez M, Spencer ML, Izzo JG, Juroske DM, Balhara K, Cody DD, et al. Inhibition of mammalian target of rapamycin reverses alveolar epithelial neoplasia induced by oncogenic K-ras. Cancer research. 2005 Apr 15;65(8):3226–3235. doi: 10.1158/0008-5472.CAN-04-4420. [DOI] [PubMed] [Google Scholar]
- 28.Granville CA, Warfel N, Tsurutani J, Hollander MC, Robertson M, Fox SD, et al. Identification of a highly effective rapamycin schedule that markedly reduces the size, multiplicity, and phenotypic progression of tobacco carcinogen-induced murine lung tumors. Clin Cancer Res. 2007 Apr 1;13(7):2281–2289. doi: 10.1158/1078-0432.CCR-06-2570. [DOI] [PubMed] [Google Scholar]
- 29.Corbett TH, Roberts BJ, Leopold WR, Peckham JC, Wilkoff LJ, Griswold DP, Jr, et al. Induction and chemotherapeutic response of two transplantable ductal adenocarcinomas of the pancreas in C57BL/6 mice. Cancer research. 1984 Feb;44(2):717–726. [PubMed] [Google Scholar]
- 30.De Angel RE, Berrigan D, Nunez NP, Hursting SD, Perkins SN. Dietary calcium source influences body composition, glucose metabolism and hormone levels in a mouse model of postmenopausal obesity. In vivo (Athens, Greece) 2009 Jul–Aug;23(4):527–535. [PubMed] [Google Scholar]
- 31.Giovannucci E, Michaud D. The role of obesity and related metabolic disturbances in cancers of the colon, prostate, and pancreas. Gastroenterology. 2007 May;132(6):2208–2225. doi: 10.1053/j.gastro.2007.03.050. [DOI] [PubMed] [Google Scholar]
- 32.Li D, Yeung SC, Hassan MM, Konopleva M, Abbruzzese JL. Antidiabetic therapies affect risk of pancreatic cancer. Gastroenterology. 2009 Aug;137(2):482–488. doi: 10.1053/j.gastro.2009.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schneider MB, Matsuzaki H, Haorah J, Ulrich A, Standop J, Ding XZ, et al. Prevention of pancreatic cancer induction in hamsters by metformin. Gastroenterology. 2001 Apr;120(5):1263–1270. doi: 10.1053/gast.2001.23258. [DOI] [PubMed] [Google Scholar]
- 34.Namba R, Maglione JE, Davis RR, Baron CA, Liu S, Carmack CE, et al. Heterogeneity of mammary lesions represent molecular differences. BMC Cancer. 2006;6:275. doi: 10.1186/1471-2407-6-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neshat MS, Mellinghoff IK, Tran C, Stiles B, Thomas G, Petersen R, et al. Enhanced sensitivity of PTEN-deficient tumors to inhibition of FRAP/mTOR. Proc Natl Acad Sci U S A. 2001 Aug 28;98(18):10314–10319. doi: 10.1073/pnas.171076798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Podsypanina K, Lee RT, Politis C, Hennessy I, Crane A, Puc J, et al. An inhibitor of mTOR reduces neoplasia and normalizes p70/S6 kinase activity in Pten+/− mice. Proc Natl Acad Sci U S A. 2001 Aug 28;98(18):10320–10325. doi: 10.1073/pnas.171060098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yu K, Toral-Barza L, Discafani C, Zhang WG, Skotnicki J, Frost P, et al. mTOR, a novel target in breast cancer: the effect of CCI-779, an mTOR inhibitor, in preclinical models of breast cancer. Endocr Relat Cancer. 2001 Sep;8(3):249–258. doi: 10.1677/erc.0.0080249. [DOI] [PubMed] [Google Scholar]
- 38.Moore T, Beltran L, Carbajal S, Strom S, Traag J, Hursting SD, et al. Dietary energy balance modulates signaling through the Akt/mammalian target of rapamycin pathways in multiple epithelial tissues. Cancer Prev Res (Phila) 2008 Jun;1(1):65–76. doi: 10.1158/1940-6207.CAPR-08-0022. [DOI] [PubMed] [Google Scholar]
- 39.Fraenkel M, Ketzinel-Gilad M, Ariav Y, Pappo O, Karaca M, Castel J, et al. mTOR inhibition by rapamycin prevents beta-cell adaptation to hyperglycemia and exacerbates the metabolic state in type 2 diabetes. Diabetes. 2008 Apr;57(4):945–957. doi: 10.2337/db07-0922. [DOI] [PubMed] [Google Scholar]
- 40.Houde VP, Brule S, Festuccia WT, Blanchard PG, Bellmann K, Deshaies Y, et al. Chronic rapamycin treatment causes glucose intolerance and hyperlipidemia by upregulating hepatic gluconeogenesis and impairing lipid deposition in adipose tissue. Diabetes. Jun;59(6):1338–1348. doi: 10.2337/db09-1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang J, Gao Z, Yin J, Quon MJ, Ye J. S6K directly phosphorylates IRS-1 on Ser-270 to promote insulin resistance in response to TNF-(alpha) signaling through IKK2. J Biol Chem. 2008 Dec 19;283(51):35375–35382. doi: 10.1074/jbc.M806480200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Harrington LS, Findlay GM, Gray A, Tolkacheva T, Wigfield S, Rebholz H, et al. The TSC1-2 tumor suppressor controls insulin-PI3K signaling via regulation of IRS proteins. J Cell Biol. 2004 Jul 19;166(2):213–223. doi: 10.1083/jcb.200403069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tremblay F, Brule S, Hee Um S, Li Y, Masuda K, Roden M, et al. Identification of IRS-1 Ser-1101 as a target of S6K1 in nutrient- and obesity-induced insulin resistance. Proc Natl Acad Sci U S A. 2007 Aug 28;104(35):14056–14061. doi: 10.1073/pnas.0706517104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ozes ON, Akca H, Mayo LD, Gustin JA, Maehama T, Dixon JE, et al. A phosphatidylinositol 3-kinase/Akt/mTOR pathway mediates and PTEN antagonizes tumor necrosis factor inhibition of insulin signaling through insulin receptor substrate-1. Proc Natl Acad Sci U S A. 2001 Apr 10;98(8):4640–4645. doi: 10.1073/pnas.051042298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yokogami K, Wakisaka S, Avruch J, Reeves SA. Serine phosphorylation and maximal activation of STAT3 during CNTF signaling is mediated by the rapamycin target mTOR. Curr Biol. 2000 Jan 13;10(1):47–50. doi: 10.1016/s0960-9822(99)00268-7. [DOI] [PubMed] [Google Scholar]
- 46.Zhang Y, Daquinag A, Traktuev DO, Amaya-Manzanares F, Simmons PJ, March KL, et al. White adipose tissue cells are recruited by experimental tumors and promote cancer progression in mouse models. Cancer research. 2009 Jun 15;69(12):5259–5266. doi: 10.1158/0008-5472.CAN-08-3444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Galie M, Konstantinidou G, Peroni D, Scambi I, Marchini C, Lisi V, et al. Mesenchymal stem cells share molecular signature with mesenchymal tumor cells and favor early tumor growth in syngeneic mice. Oncogene. 2008 Apr 17;27(18):2542–2551. doi: 10.1038/sj.onc.1210920. [DOI] [PubMed] [Google Scholar]
- 48.Muehlberg FL, Song YH, Krohn A, Pinilla SP, Droll LH, Leng X, et al. Tissue-resident stem cells promote breast cancer growth and metastasis. Carcinogenesis. 2009 Apr;30(4):589–597. doi: 10.1093/carcin/bgp036. [DOI] [PubMed] [Google Scholar]
- 49.Trayhurn P, Wood IS. Signalling role of adipose tissue: adipokines and inflammation in obesity. Biochem Soc Trans. 2005 Nov;33(Pt 5):1078–1081. doi: 10.1042/BST0331078. [DOI] [PubMed] [Google Scholar]
- 50.Subbaramaiah K, Howe LR, Bhardwaj P, Du B, Gravaghi C, Yantiss RK, et al. Obesity is associated with inflammation and elevated aromatase expression in the mouse mammary gland. Cancer Prev Res (Phila) 2011 Mar;4(3):329–346. doi: 10.1158/1940-6207.CAPR-10-0381. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 51.Hursting SD. Inflammatory Talk: Linking Obesity, NF-{kappa}B, and Aromatase. Cancer Prev Res (Phila) 2011 Mar;4(3):285–287. doi: 10.1158/1940-6207.CAPR-11-0056. [DOI] [PubMed] [Google Scholar]