Abstract
Background
Patients with cancer frequently visit the emergency department (ED) and are at high risk for hospitalization due to severe illness from cancer progression or treatment side effects. With an aging population and rising cancer incidence rates worldwide, it is crucial to understand how EDs and other acute care venues manage oncologic emergencies. Insights from other nations and health systems may inform resources necessary for optimal ED management and novel care delivery pathways. We described clinical management of oncologic emergencies and their contribution to ED visits and hospitalizations worldwide.
Methods
We performed a systematic review of peer-reviewed original research studies published in the English language between January 1st, 2003, to December 31st, 2022, garnered from PubMed, Web of Science, and EMBASE. We included all studies investigating adult (≥ 18 years) cancer patients with emergency visits. We examined chief complaints or predictors of ED use that explicitly defined oncologic emergencies.
Results
The search strategy yielded 49 articles addressing cancer-related emergency visits. Most publications reported single-site studies (n = 34/49), with approximately even distribution across clinical settings- ED (n = 22/49) and acute care hospital/ICU (n = 27/49). The number of patient observations varied widely among the published studies (range: 9 – 87,555 patients), with most studies not specifying the cancer type (n = 33/49), stage (n = 41/49), or treatment type (n = 36/49). Most studies (n = 31/49) examined patients aged ≥ 60 years. Infection was the most common oncologic emergency documented (n = 22/49), followed by pain (n = 20/49), dyspnea (n = 19/49), and gastrointestinal (GI) symptoms (n = 17/49). Interventions within the ED or hospital ranged from pharmacological management with opioids (n = 11/49), antibiotics (n = 9/49), corticosteroids (n = 5/49), and invasive procedures (e.g., palliative stenting; n = 13/49) or surgical interventions (n = 2/49).
Conclusion
Limited research specifically addresses oncologic emergencies despite the international prevalence of ED presentations among cancer patients. Patients with cancer presenting to the ED appear to have a variety of complaints which could result from their cancers and thus may require tailored diagnostic and intervention pathways to provide optimal acute care. Further acute geriatric oncology research may clarify the optimal management strategies to improve the outcomes for this vulnerable patient population.
Keywords: Emergency department, Acute care, Oncologic emergencies, Systematic review, Older adults
Introduction
Patients with cancer are frequent users of the emergency department (ED), often incurring multiple visits per patient in a given year [1–3]. Approximately one-third of patients with cancer have unplanned ED visits and hospitalizations for symptom management of oncologic emergencies [4], including pain, dyspnea, infection, nausea or vomiting, and other disease- and treatment-related complications [5, 6]. Patients with cancer present to the ED with high triage acuity, many of whom exhibit other comorbidities, thus requiring particularly complex care coordination [7–9]. Case complexity may particularly motivate ED visits, as unique constellations of social determinants, clinical conditions, health care infrastructure, and local/regional/federal policy interactions may encourage urgent care seeking [9, 10]. In the US, among patients with cancer, higher ED usage is associated with non-White and African American race/ethnicity, older age, male gender, Medicaid or uninsured status, and receipt of < 100 days of palliative care in advanced cases [9, 11]. Additionally, studies observe a diagnosis of depression, comorbidities, combinations of cancer treatments, delays to treatment initiation, and end-of-life (EOL) predict ED visit frequency with a greater proportion of encounters resulting in admission (58–62%) compared to the general population [9, 10, 12–17]. The ED, required to address a spectrum of conditions and acuteness, is a centralized setting that frequently provides care for patients with oncologic emergencies.
EDs are essential to addressing patients’ acute medical needs, yet the structure, financing, and resources of acute unscheduled care delivery vary. In the US, settings range from highly resourced, large-volume (> 50,000 annual visits) urban EDs of tertiary academic medical centers to smaller community-based rural EDs [18, 19]. Internationally, systems of emergency medicine (EM) differ vastly. For example, the National ED Inventories (NEDI) project analyzed EDs in Beijing, China, and Quito, Ecuador; the study revealed all surveyed sites were located in a hospital, with the majority having a contiguous layout (i.e., providing medical and surgical care in one area) and triage to service (i.e., ED patients directed to emergency care from non-EM specialties) [20, 21]. Conversely, many Slovenian EDs are non-hospital-based (i.e., located in health centers rather than a hospital) and may be within other specialty units [19, 22]. Despite these different settings, most EDs report a contiguous design, with only 39% using triage to service [19, 22]. Apart from structural variation, disparities in resources exist across the world [23, 24]. Despite international differences, EDs across the globe share the prevalence of high frequency of ED use among patients with cancer [9, 25–27]. Essentially, EDs worldwide face oncologic emergencies subject to the ED’s native infrastructure, practice culture, and community policy.
An international increase in cancer cases underscores the need for care assessment and improvement in oncologic emergency treatment. Therefore, we undertook a systematic review to describe the global management of common oncologic emergencies and related hospital care.
Materials and methods
Study design
We conducted a systematic review of the literature, which was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [28].
Eligibility criteria
We included original research articles that examined oncological emergencies and interventions. We included all cancer types and did not require the publications to articulate strict diagnostic criteria or treatment interventions. We excluded non-English-language publications.
Search strategy
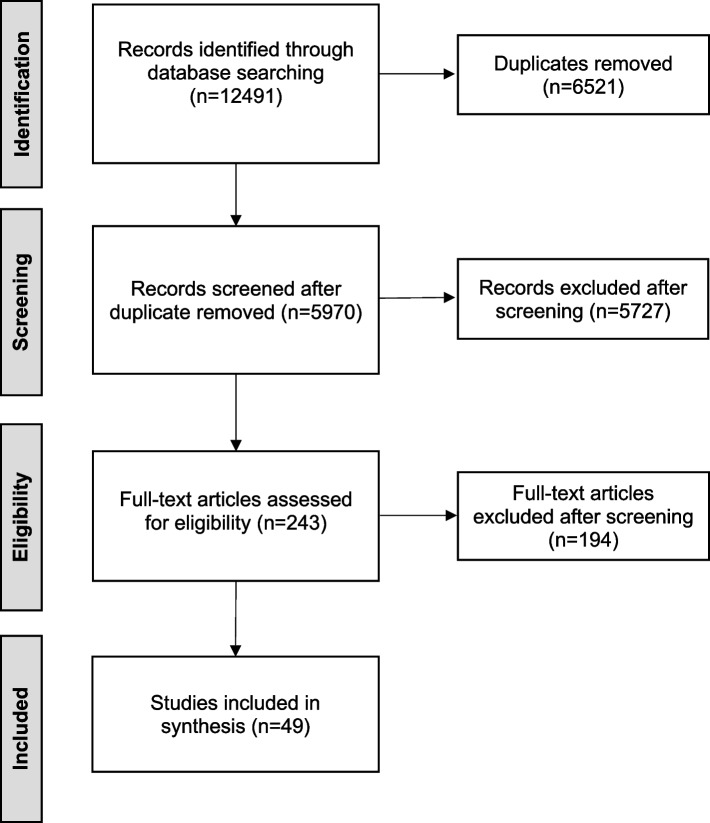
Figure 1 illustrates the detailed search strategy. We searched PubMed, Web of Science, and EMBASE healthcare databases for literature published between January 1st, 2003, to December 31st, 2022. A liaison librarian (JM), in collaboration with the research team, developed the publication search strategy to identify publication abstracts corresponding to the following Medical Subject Headings (MeSH) and keywords: oncologic emergencies, emergency medicine, acute care, and cancer. This search strategy was adapted for each database (e.g., EMBASE). A second liaison librarian (DC) performed a peer review of electronic search strategies (PRESS) to refine the search further. Investigators applied the refined search strategy to additional databases which identified 12,491 citations. Investigators imported these results in Covidence (https://www.covidence.org), a web-based software platform for conducting systematic reviews that additionally eliminates duplicate records
Fig. 1.
Detailed search strategy for each database
Study selection
Studies were included if they were (1) empirical, peer-reviewed original research, (2) focused on adult (≥ 18 years) patients with cancer, (3) on cancer as a primary disease in the ED, ICU, hospital, other urgent or acute care settings, (4) included chief complaints at ED or predictors of ED use and had explicitly defined oncologic emergencies [4]. Investigators excluded: (1) abstracts, literature reviews, editorial reviews/commentaries, conceptual papers, or case reports; (2) studies that explored pediatric populations (as part of or the entire sample), and (3) referenced oncologic emergencies without subsequent clinical address or care focus. A group of 12 reviewers (SY, AH, KA, JK, NW, MH, JB, MW, BGR, SH, CRG, CC) screened records from the initial search of the databases and agreed on studies for inclusion. Each record underwent an initial title/abstract screening and a subsequent full-text screening, with each reference reviewed by at least two coders. The research team resolved discrepancies or ambiguities in coding during consensus meetings.
Data extraction and analysis
A study-specific abstraction coding sheet was developed a priori. The study design, country where the study was conducted, number of sites, whether it was an ED or any other acute care setting (e.g., ICU), number of patients, cause of the ED visit/hospitalization (i.e., oncologic emergency specified), intervention(s) used to treat that oncologic emergency, and the outcomes studied were abstracted. Other extracted data included aim and objectives, methods, study population, nature of oncologic emergencies and intervention used in the ED/hospital, outcome measures, results, and conclusions. Given our focus on various types of empirical studies and the exploratory nature of this review, quality assessment was not performed. However, studies were included only if the publication reported specific oncologic emergencies and/or interventions used in the ED. Figure 2 illustrates the review process.
Fig. 2.
PRISMA flow diagram
Results
Description of studies
Table 1 notes study characteristics and Table 2 describes the articles in detail [29–77]. The search strategy identified 12,491 citations about cancer-related emergency visits, of which 49 met inclusion criteria (Fig. 2): 28 retrospective cohort studies, 13 prospective cohort studies, four randomized controlled trials (RCTs), three cross-sectional, and one case–control design. Of the papers reviewed, 18 originated from the Americas, 13 were from Europe, 12 were from Asian countries, two from Australia, and four from multi-national studies (Fig. 3). Most studies were conducted in a single site (n = 34/49), with comparable proportions of ED visits (n = 22/49) and acute care hospital/ICU visits (n = 27/49). The study population size varied widely among the identified studies (range 9 – 87,555 participants), with most studies not specifying the cancer type, stage, or treatment types, and over 63% of studies had an average age ≥ 60 years. The earliest publication meeting the study criteria appeared in 2003, with 84% of the remaining papers published after 2010.
Table 1.
Demographics and clinical characteristics of studies (n = 49)
| Age in Years (Median or Mean as reported) | ||
|---|---|---|
| < 60 | 12 | |
| 60–64 | 10 | |
| 65–69 | 15 | |
| 70 + | 6 | |
| Age Range not reported | 6 | |
| Cancer Type | Specific cancer type | 8a |
| Hematological | 4 | |
| Solid | 4 | |
| Cancer type not specified | 33 | |
| Cancer Stage | Advanced | 8 |
| Cancer stage not specified | 41 | |
| Treatment Type | Chemotherapy | 7 |
| Immunotherapy | 3 | |
| Radiotherapy | 1 | |
| Surgery | 2 | |
| Treatment type not specified | 36 |
aThere were two studies on colorectal cancer, four on lung cancer, one on lymphoma, and one on prostate cancer
Table 2.
Detailed description of studies included (n = 49)
| Author, year | Country | Methods | Population | Sample Size | Age, years (Mean, SD, or Median) | % Male | Cancer Studied | Oncologic Emergency Studied | Intervention Used in the ED/Hospital |
|---|---|---|---|---|---|---|---|---|---|
| Abelson et al., 2017 [29] | United States | Retrospective Observational Cohort Study | Patients admitted to the ED with MLBO who were treated with palliative stent (n = 172) or stoma (n = 173) | 345 | 69.9 (14.4) (stoma group), 70.9 (16.8) (stent group) | 87 (50.3%, stoma); 90 (52.3% stent) | Colorectal | palliation of malignant large-bowel obstruction (MLBO) | Palliative stenting or stoma creation |
| Alsirafy et al., 2016 [30] | Other: Egypt | Retrospective Observational Cohort Study | Patients with terminal cancer who died at KAMC-HC during the 13-month period | 154 | Median (range): 60 (16–91) | 69 (44.8%) | All | Pain, dyspnea, vomiting | n/a |
| Azoulay et al., 2021 [31] | Other: France, Spain, USA, UK, Russia, Canada, Germany, Austria | Retrospective Observational Cohort Study | Patients who received CAR T-cell therapy in the past 30 days had been admitted to the ICU for any reason | 241 | Median (range): 58 (43–66) | 144 (60%) | All hematological malignancies | Isolated cytokine release syndrome, sepsis (due to pneumonia, enterocolitis, and skin and soft tissue infections), frailty | Life-saving treatments (vasoactive drugs), non-invasive ventilation or high-flow nasal oxygen, steroid therapy, |
| Banala et al., 2020 [32] | United States | Randomized Clinical Trial | Adult patients with cancer presenting with severe pain to the ED | 84 | Median (range): IV Hydromorphone group: 51 (29–78); Intranasal Fentanyl group)55 (22–84) | 36 (43.9%) | All | Severe pain | Intranasal fentanyl (INF) vs intravenous hydromorphone (IVH) |
| Bosscher et al., 2016 [33] | Other: The Netherlands | Prospective Observational Cohort Study | Adult cancer patients (age [18 years) in the University Medical Center Groningen who required surgical consultation for oncologic emergencies | 207 | Not reported | 101 (48.8%) | All | Obstruction, infection, clinical deterioration, gastrointestinal perforation, bleeding/thrombosis, pathological fractures | Referral to surgery within 30 days after emergency evaluation or non-surgical treatment |
| Bou Chebl et al., 2021 [34] | Other: Lebanon | Retrospective Observational Cohort Study | All patients > 18 years of age admitted with sepsis | 442 | 67.92 (13.32, solid tumor); 55.37 (20.85, hematological malignancy) | 190 (62.3% solid); 97 (70.8% hematological) | All | Sepsis | IV fluids, Vasopressor use, steroid use, intubation |
| Bow et al., 2006 [35] | Other: USA, Canada, Australia | Randomized Clinical Trial | Patients at high risk for medical complications who were > = 18 years old, severely neutropenic, hospitalized for the management of a febrile episode complicating the course of cytotoxic therapy for a hematological malignancy or for a hematopoietic stem cell transplant (HSCT), and who had provided written, informed consent according to institutional protocol | 264 | 50.2 (15.1, Piperacillin-tazobactam recipients); 50.1 (14.5, Cefepime recipients) | 166/265 (62.6% Piperacillin-tazobactam recipients); 146/263 (54.4% Cefepime recipients) | All Hematological malignancies | Febrile neutropenic episodes | n/a |
| Castillo et al., 2021 [36] | United States | Retrospective Observational Cohort Study | Patients receiving ICI therapy within 6 weeks before ED presentation who had a contemporary evaluation in the Mayo Clinic Hospital ED between May 1, 2017, and April 30, 2018 | 67 | Median (range): 65 (24–88) | 36 (53.7%) | All | Immune-related adverse events (abdominal pain, colitis, diarrhea, hyperglycemia, shortness of breath, dizziness, chest pressure/tightness, nausea and vomiting) | Corticosteroids (dexamethasone 10 mg, prednisone 60 mg) |
| Cauley et al., 2015 [37] | United States | Retrospective Observational Cohort Study | Patients included in this study were at least 18 years old, had a preoperative diagnosis of disseminated cancer and Patients who underwent an emergency operation for intestinal obstruction or perforation by the primary DRG International Classification of DiseasesV9th Rev. (ICD-9) code | 875 | Not reported | 52% (in intestinal perforation group); 51% (in Obstruction group) | All | Intestinal Obstruction or Perforation | Emergency Operation |
| Chou et al., 2012 [38] | Other: Taiwan | Retrospective Observational Cohort Study | Consecutive patients with stage III to stage IV lung cancer, who were admitted to ICU for sepsis-related respiratory failure | 70 | 71.7 (12.3, survived to hospital discharge); 76.4 (11.6, died) | 23 (79.3% survived to hospital discharge); 37 (90.2% died) | Lung, stage III and IV | Sepsis-related respiratory failure | Intubated via mechanical ventilator support. If patients failed to be weaned from the ventilator, they were transferred to a respiratory care facility for long-term ventilator support |
| Cooksley et al., 2020 [39] | UK | Prospective Observational Cohort Study | All emergency presentations in patients treated with ICIs within 6 months before admission were seen at a specialist oncology hospital in England from 20th May 2018 to 19th May 2019 | 300 | Median (range): 67 (28–88) | 185 (61.7%) | All | Dyspnea, diarrhea, and fever related to ICI toxicity | Steroids, antibiotics |
| Coyne et al., 2021 [40] | United States | Prospective Observational Cohort Study | Adults 18 years or older with active cancer presenting to the ED | 1075 | Median (range): 64 (19–90) | 518 (48.2%) | All | Pain | Opioids, acetaminophen |
| Delgado-Guay et al., 2015 [41] | United States | Retrospective Observational Cohort Study | Patients with advanced cancer aged 18 years or older who visited the ED after their first visit to an outpatient palliative care clinic | 200 | 56.5 (13.6) | 104 (52%) | All | pain, GI symptoms, altered mental status, other neurologic symptoms, infection, dyspnea, fever/chill, bleeding, edema/swelling, constipation, general weakness, fell down | received palliative care consultation in the ED or admitted to the hospital |
| DeSilva, Jackson, and Steer, 2018 [42] | Australia | Retrospective Observational Cohort Study | Patients ≥ 18 years of age who were admitted under the oncology unit at Albury Wodonga Health during a 12-month period and who had a microbiological test performed for suspected infection during their admission | 208 | Median (range): 67 (19–89, with febrile neutropenia); 68 (19–89, without febrile neutropenia) | 28 (56% with febrile neutropenia); 99 (62.7%, without febrile neutropenia) | All | Infection, neutropenic fever episodes | Antibiotic therapy |
| Frago et al., 2010 [43] | Other: Spain | Retrospective Observational Cohort Study | Patients with stage IV obstructing CRC presenting to the ED | 55 | 65.5 (50–77, surgery group); 65.9 (19–84, stent group) | 9/12 (75% surgery group); 32/43 (74.41%, stent group) | Colorectal, stage IV | Bowel obstruction | Colonic stenting or palliative chemotherapy (consisting of a combi-nation of 5-fluorouracil (5-FU), leucovorin (LV), and irino-tecan (FOLFIRI) or oxaliplatin (FOLFOX)) |
| Giustozzi et al., 2021 [44] | Other: Italy, USA, Belgium, France, Germany, Israel, Netherlands, UK, Poland, and Spain | Randomized Clinical Trial | Patients with cancer with symptomatic or incidental acute proximal deep vein thrombosis or pulmonary embolism were randomized in a 1:1 ratio to receive oral apixaban or subcutaneous dalteparin | 1155 | 67.3 (11.0, incidental VTE); 68 (11.2, Symptomatic VTE) | 115 (50%, incidental VTE); 453 (49%, symptomatic VTE) | All | Incidental or symptomatic acute proximal deep venous thromboembolism (VTE) | Lab testing, diagnostic imaging |
| Grewal et al., 2020 [45] | Canada | Retrospective Observational Cohort Study | Patients aged 18 years and older with a cancer diagnosis and who received chemotherapy in the 30 days before being seen in an emergency department between 2013 and 2017 | 87,555 | 66 (56–74) | 39,383(45%) | All | Infection, fever, gastrointestinal diagnoses | Specialty consultation, hospital admission |
| Gudiol et al., 2016 [46] | Other: Spain | Prospective Observational Cohort Study | Advanced solid neoplasm was considered in patients with confirmed metastatic disease (stage IV) and some tumors in stage III (lung, pancreas, gastric, esopha-geal and urothelial) not suitable for curative treatment | 795 | 64 (29–89) | 35 (63.6%) | All | Bacteremic pneumonia in neutropenic cancer patients, fever, cough, septic shock, | ICU admission, invasive mechanical ventilation, antibiotic therapy, targeted antibiotic therapy |
| Hsu et al., 2021 [47] | Other: Taiwan | Retrospective Observational Cohort Study | Adults with cancer who received palliative care during the final 6 months of their life | 762 | 70.4 (13.0) | 44 (49.4%) | All | Anemia, altered mental status, catheter-related events, dyspnea, falls, fever, N/V or other GI symptoms, pain, and tumor bleeding/complications | n/a |
| Kao et al., 2018 [48] | Other: Taiwan | Case–Control Study | Advanced cancer patients receiving palliative home care services | 65 | 72.6 (12.1) | 35 (54.8) | All | Pain, infection or fever, nausea or vomiting, constipation, dyspnea, change of consciousness, and gastrointestinal bleeding | Morphine |
| Kerhuel et al., 2015 [49] | Other: France | Retrospective Observational Cohort Study | All patients admitted to the ICU within the 3 months following HDT/ASCT during the study period | 27 | 54 (38–60) | 14 (52%) | Lymphoma | Infection, shock, acute respiratory failure, neurologic disorder, bleeding | Vasopressors, invasive mechanical ventilation, non-invasive mechanical ventilation, renal replacement therapy |
| Kim et al., 2014 [50] | Other: Korea | Retrospective Observational Cohort Study | Patients with pathologically confirmed lung cancer who were admitted to the medical ICU at Seoul National Uni-versity Bundang Hospital between 2003 and 2011 | 95 | 65.6 (10.3) | 78 (82%) | Lung, stage IIIB and IV | Obstructive pneumonia, respiratory failure due to lung involvement of cancer, cardiac tamponade, tumor bleeding, neurologic events, metabolic events, radiation pneumonitis, chemo-induced lung toxicity, infection with neutropenia, infection without neutropenia, other complications due to treatment, neutropenic septic shock, comorbidity related events | Vasoactive agents, hemodialysis, CPR, mechanical ventilation |
| Klamroth et al., 2022 [51] | Other: Germany | Prospective Observational Cohort Study | Patients diagnosed with cancer-associated venous thrombosis with newly diagnosed symptomatic or asymptomatic VTE, pulmonary embolism (PE), or deep vein thromboses (DVT) and age ≥ 18 years | 382 | Median is 67 years for patients with CAT | 189 (49.5%, patients with CAT) | All | Cancer-associated venous thrombosis (CAT) | Anticoagulant therapy with low-molecular weight heparin, direct oral anticoagulants, Vit K antagonists, unfractionated heparin |
| Lagman et al., 2007 [52] | United States | Prospective Observational Cohort Study | Patients who were admitted to The Harry R. Horvitz Acute Inpatient Palliative Medicine Unit with an episode needing acute inpatient treatment for symptom control or management of complications | 96 | 62 (31–92) | 48 (50%) | All | Acute inpatient treatment of symptom control and cancer-related complications (i.e., neutropenic fever, radiation-induced pneumonitis, intractable emesis), terminal care, antineoplastic therapy-induced complications, comorbid condition related symptoms | Invasive diagnostic (i.e., endoscopy) and therapeutic procedures, medications (i.e., opioids, laxatives, acid suppressants, corticosteroids, antiemetics), hydration, transfusions, radiation or chemo or a combination, discharged home with hospice care, lab tests, radiologic investigations |
| Mercadante et al., 2010 [53] | Other: Italy | Prospective Observational Cohort Study | Patients consecutively admitted to a Pain Relief and Palliative Care unit in a period of 6 months from January 2008 to June 2008, who were receiving opioids in doses of oral morphine equivalents equal to or more than 60 mg daily or who were prescribed opioids for breakthrough pain (BTP) of different nature | 66 | 66.7 (12.2) | 42 (63.6%) | All | Pain | Opioids intravenous, oral, transdermal |
| Mercadante et al., 2017 [54] | Other: Italy | Prospective Observational Cohort Study | Advanced cancer patients who were admitted to an APSCU | 235 | 66.7 (11.9, first admission); 62.7 (11.9, readmission) | 134 (57%, first admission); 48 (60.8% readmissions) | All | Uncontrolled pain, opioid-induced toxicity, chemotherapy-induced toxicity, symptom control, and end-of-life care | Opioid therapy |
| Miranda et al., 2016 [55] | Other: Brazil | Cross-Sectional Study | Patients with cancer treated at oncological service and attended an ED for oncologic monitored from September 2011 to December. 2011, with length of stay > 2 h, aged 18 years or older | 191 | Not reported | 68 (35.6) | All | Infection, pain, GI symptoms, respiratory symptoms, | n/a |
| Moghnieh et al., 2015 [56] | Other: Lebanon | Retrospective Observational Cohort Study | Adult cancer patients with fever and neutropenia, including those undergoing Hematopoietic Stem Cell Transplantation (HSCT), with positive blood cultures were selected | 70 | Not reported | 36 (48%) | All | Febrile neutropenia | n/a |
| Numico et al., 2015 [57] | Other: Italy | Retrospective Observational Cohort Study | Patients admitted to the General Valle d’Aosta Hospital inpatient oncology ward between August 1, 2011 and December 31 2012 | 454 | 69.2 (26–92) | 258 (56.9%) | All | Breathlessness, pain, fever, intestinal obstruction, other digestive symptoms (nausea and vomiting, jaundice, diarrhea, dysphagia, etc.), neurological symptoms (mainly related to brain metastases or meningeal carcinomatosis), general symptoms (such as fatigue and cachexia) and cardiovascular symptoms (such as those related to deep vein thrombosis, pericardial effusion, heart failure) | Imaging, antitumor interventions, antibiotics, opiates, diagnostic or therapeutic invasive procedures (thoracentesis for pleural effusion or biliary drainage for obstruction), chemotherapy or radiotherapy, transferred to hospice, or in-hospital death |
| Patel et al., 2017 [58] | United States | Retrospective Observational Cohort Study | Opioid-tolerant cancer patients > 18 years old who presented to two urban tertiary-care EDs between January 1, 2012 and November 30, 2014 and received opioids for the management of acute pain | 216 | Mean (range): 58 (29–89) | 92 (42.40%) | All | Pain | Opioids |
| Peyrony et al., 2021 [59] | Other: France | Cross Sectional Study | Patients of 18 years or older with solid or hematologic malignancy | 1081 | 72 (62–82) | 611 (56.52%) | All | Dyspnea, neurological disorder, and fatigue | Ultrasound, blood tests, ECG, venous access, oxygen therapy, mechanical ventilation, existing tracheostomy use, fluid challenge, catecholamines, analgesia, morphine, CPR, sedation, antibiotics, |
| Poutsiaka et al., 2007 [60] | United States | Prospective Observational Cohort Study | All patients receiving daptomycin resided on the Bone Marrow Transplant Units of the two participating institutions (Tufts-New England Medical Center, Boston Massachusetts and the University of Iowa Hospital, Iowa City, Iowa) from 2000 to 2002 | 9 | Mean (range): 52.9 (25–70) | 7/9 (77.8%) | All hematological malignancies | Treating VRE BSI in febrile neutropenic patients | Daptomycin |
| Raghavendra et al., 2014 [61] | United States | Retrospective Observational Cohort Study | Patients with neutropenic fever with fever > 38.8 degrees Celsius | 215 | Median is 69 years | Not reported | All | Neutropenic fever | Antibiotics and infectious disease consult service use |
| Rolston et al., 2010 [62] | United States | Prospective Observational Cohort Study | Patients with neutropenic fever | 21 | 44 (24–84) | 4 (19%) | All solid tumors | Neutropenic fever | Physical exam, lab tests, oral moxifloxacin |
| Ruiz-Artacho et al., 2018 [63] | Other: USA, Argentina, Austria, Belgium, Brazil, China, Colombia, Czechia, Ecuador, Egypt, France, Germany, Greece, Honduras, Iran, Ireland, Israel, Italy, Japan, Latvia, Morocco, North Macedonia, Portugal, Spain, Switzerland, UK, Vietnam, | Prospective Observational Cohort Study | Patients with biopsy-proven active cancer in the lung presenting with acute symptomatic, objectively confirmed VTE | 1725 | 65 (12.0, both pulmonary embolism and deep VT groups) | 873 (72%, Pulmonary embolism); 377 (73%, Deep VT) | Lung | Recurrent DVT, or PE and major bleeding | Anticoagulant therapy, repeat compression ultrasonography, helical CT pulmonary, ventilation–perfusion lung scintigraphy, angio-graphy, or pulmonary angiography |
| Sandgren et al., 2010 [64] | Other: Sweden | Cross Sectional Study | Palliative cancer patients | 520 | 70 (62, 71, 79 quartiles, 2002 DATA); 74 (67, 76, 83, 2007) | 107 (55.7%, 2002); 182 (55.5%, 2007) | All | Pain, deterioration, nausea, infection | n/a |
| Skiba et al., 2020 [65] | Australia | Retrospective Observational Cohort Study | Adult cancer patients with a recorded diagnosis of neutropenic fever who were hospitalized at a tertiary care hospital between January 2017 and December 2017 | 88 | 64 (12.25) | 31 (35.2) | All solid tumors | Neutropenic fever | Antibiotics |
| Soares, Martins, and Uchoa, 2003 [66] | Other: Brazil | Prospective Observational Cohort Study | Patients with severe cancer pain admitted to our palliative care center’s emergency room between April 2001 and June 2002 and aged between 18 and 80, on concurrent morphine therapy for at least 2 weeks, and had severe pain at initial assessment | 18 | 51 (34–74) | 10 (55.5%) | All solid tumors | Severe pain | IV fentanyl |
| Sutradhar, Barbera, and Seow, 2017 [67] | Canada | Retrospective Observational Cohort Study | Each decedent had to be at least 18 years of age at cancer diagnosis and had to have received homecare nursing (with standard or palliative intent) prior to their date of death | 54,743 | Not reported | 26,913 (47.9%) | All | Dyspnea, malaise and fatigue, acute abdominal or pelvic pain, fever with chills, pain in throat, projectile vomiting, nausea, disorientation, rheumatism or other soft-tissue disorders, panniculitis affecting regions of next and back multiple sites in spine | n/a |
| Teimouri et al., 2022 [68] | Canada | Retrospective Observational Cohort Study | Adult medical oncology patients (≥ 18 years of age) with an NSH-CZ postal code who had received at least one dose of nivolumab, ipilimumab, or the nivolumab plus ipilimumab combination for cancer treatment at the Victoria General Hospital | 129 | 64 (11.0) | 84 (65.1%) | All | Diarrhea/colitis, hepatitis, pneumonitis, nephrotoxicity, and cardiotoxicity | Steroids |
| Verhoef et al., 2020 [69] | Other: Netherlands | Retrospective Observational Cohort Study | Adult patients who visited the ED between May 2011 and June 2014, included those who were in the palliative phase of cancer at the moment of the ED visit and died within 3 months thereafter | 420 | 63 (22–92) | 229 (54.5%) | All | Dyspnea, pain, and ascites | Imaging and blood tests, EOL goals of care discussions, hospitalizations |
| Verhoef et al., 2020 [70] | Other: Netherlands | Retrospective Observational Cohort Study | All adult patients with HM who died within 3 months after their last ED visit were included. They were compared to patients. with ST having advanced cancer, which was defined as not having any curative options or receiving anticancer treatment not aimed at curation | 498 | 63 (22–94, all); 61 (27–94, HM); 61 (22–92, ST) | 282 (56.6%, all); 53/78 (67.9%, HM); 229/420 (54.5%, ST) | All | Dyspnea, pain, fever, nausea or vomiting, neurologic deterioration, weakness or loss of strength, bleeding, obstipation or diarrhea, fatigue, difficulty swallowing or passage problems, seizure, edema, ascites | Diagnostic imaging, laboratory tests, hospitalization |
| Waddle et al., 2015 [71] | United States | Retrospective Observational Cohort Study | Cancer patients who initiated external beam RT at the University of North Carolina at Chapel Hill from January 1, 2010, through December 31, 2010 | 1116 | Not reported | 534 (47.85%) | All | GI symptoms, neurologic symptoms, respiratory symptoms, pain, fever or infection | n/a |
| Won et al., 2014 [72] | Other: Korea | Retrospective Observational Cohort Study | Patients aged 20 years and older, who stayed in the CED for more than 24 h and experienced pain with self-reported numeric rating scale (NRS) scores of 4 or greater at the time of admission or during the CED stay | 455 | 53.9 (11.9, before CPCP); 56.2 (11.4, after CPCP) | 81 (50%, before CPCP); 159 (55%, after CPCP) | All | Pain | Regular, time-release analgesics and immediate-release analgesics |
| Woon et al., 2021 [73] | Canada | Retrospective Observational Cohort Study | All men aged 66 and older who received abiraterone or enzalutamide as first-line (chemotherapy-naïve) treatment for mCRPC between January 1, 2012, and December 31, 2017 in Ontario, Canada | 3405 | 78.9 (7.2 overall) | 3405 (100%) | Prostate | UTI, treatment-related toxicity | n/a |
| Xia and Wang, 2016 [74] | Other: China | Retrospective Observational Cohort Study | Patients aged ≥ 18 years; medical patients with a definite diagnosis of solid cancer according to pathological results obtained by surgical or micro-invasive biopsy; tumor metastasis assessed by radiography or exfoliative cytology; life expectancy evaluated by an oncologist as > 3 months; > 3 days in the ICU; and nonpregnant women | 141 | 63 (54–74) | 87 (61.7%) | All solid tumors | Respiratory failure, severe sepsis or septic shock, acute renal failure, acute heart failure | Vasopressors, mechanical ventilation, renal replacement therapy |
| Yaman et al., 2022 [75] | Other: Turkey | Prospective Observational Cohort Study | Patients 18 years or older, having hematological cancer, having laboratory TLS or clinical TLS, and receiving a single dose (7.5 mg) rasburicase | 82 | 64 (19–85) | 43 (52.4%) | All hematological malignancies | Tumor lysis syndrome (TLS) | Rasburicase administration |
| Yildirim and Tanriverdi, 2014 [76] | Other: Turkey | Retrospective Observational Cohort Study | Patients > 18 yrs of age with cancer treated or followed at the Department of Medical Oncology of our institution between August 2011 and September 2013 | 107 | 51 (11.0, group 1); 52 (13.0, group 2) | 41 (64%, group 1); 21 (49%, group 2) | All | Dyspnea, pain, deterioration in general health status, fever, hemorrhage, icterus, abdominal distention/ascites, neurological symptoms | Pain treatment (fentanyl vs. tramadol vs. morphine), discharged, died in the ED, hospitalized |
| Yilmaz et al., 2017 [77] | Other: Turkey | Randomized Clinical Trial | Adults 18 to 65 years of age presenting to the ED with lung cancer and dyspnea; presentation to the ED with the complaint of shortness of breath and, such as dyspnea on exertion, wheezing, and accessory muscle use; not requiring assisted ventilation, peak expiratory flow rate (PEFR) of < 250 | 91 | Mean (95%CI): 54.7 (51.8–57.7) | 46 (50.5%) | Lung | Dyspnea | Salbutamol and magnesium sulfate |
Abbreviations: ED Emergency Department, MLBO Malignant large-bowel obstruction, KAMC-HC King Abdullah Medical City Health Clusters, CAR Chimeric Antigen Receptor, ICU Intensive Care Unit, IV Intravenous, INF Intranasal Fentanyl, IVH Intravenous Hydromorphone, HSCT Hematopoietic Stem Cell Transplant, ICI Immune Checkpoint Inhibitors, ICD-9 International Classification of Diseases V9th Rev., GI Gastrointestinal, CRC Colorectal Cancer, VTE Venous Thromboembolism, HDT High-dose Therapy, ASCT Autologous Stem Cell Transplant, PE Pulmonary Embolism, DVT Deep Vein Thromboses, CAT Cancer-associated Venous Thrombosis, BTP Breakthrough Pain, APSCU Acute Palliative-Supportive Care Unit, ECG Electrocardiogram, CPR Cardiopulmonary Resuscitation, VRE Vancomycin-Resistant Enterococcus, BSI Blood Stream Infection, EOL End of Life, HM Hematemesis and Melena, CED Coverage with Evidence Development, NRS Numeric Rating Scale, UTI Urinary Tract Infection, TLS Tumor lysis Syndrome
Fig. 3.
Location of Studies Included (Note: total number is greater than the sample size due to multi-country studies being listed individually)
Oncologic emergencies
The most common oncologic emergencies or predictors of ED use/hospitalization included infection (n = 22/49), pain (n = 20/49), dyspnea or respiratory symptoms (n = 19/49), gastrointestinal (GI) symptoms, including bowel obstructions (n = 17/49), and treatment-related toxicities (n = 13/49). Interventions within the ED or hospital ranged from pharmacological management with opioids (n = 11/49), antibiotics (n = 9/49), corticosteroids (n = 5/49), and invasive procedures (e.g., palliative stenting; n = 13/49) or surgical interventions (n = 2/49).
Management of infection
Infections included sepsis, febrile neutropenia, and pneumonia. Isolated cytokine release syndrome and sepsis caused by pneumonia, enterocolitis, and skin infections in patients with hematological malignancies were managed with life-saving treatments such as vasoactive drugs, non-invasive ventilation, and corticosteroid therapy [31]. Bou Chebl et al. [34] also addressed sepsis, utilizing interventions including IV fluids, vasopressors, and intubation. Some studies which focused on febrile neutropenia in patients with hematological malignancies [35, 56]did not specify ED interventions, while other studies [42, 65] highlighted antibiotic therapy as a crucial treatment. In patients with bacterial pneumonia, Gudiol et al. (2016) [46] noted the necessity for ICU admission, mechanical ventilation, and targeted antibiotic therapy. Additionally, Grewal et al. [45] emphasized the need for specialty consultations and hospital admissions for infections in cancer patients.
Addressing pain
Pain is a common and debilitating symptom in oncological emergencies, often managed with various analgesic strategies. Mercadante et al. (2010, 2017) [53, 54] reported on the management of pain using opioids such as intravenous morphine, oral morphine, transdermal fentanyl, and oral oxycodone. When comparing the efficacy of intranasal fentanyl (INF) versus intravenous hydromorphone (IVH) for severe pain relief, they report that IVH provided superior pain management [32]. Coyne et al. (2021) [40] and Patel et al. (2017) [58] both discussed opioid therapy for pain management, with Coyne et al. (2021) [40] also mentioning acetaminophen as an adjunct treatment. The use of various medications, including opioids and corticosteroids, provided acute symptom management [52]. When explicitly addressing the palliation of malignant large-bowel obstruction in colorectal cancer, palliative stenting or stoma creation was used by Abelson et al. [29]
Assessment of dyspnea and respiratory symptoms
Dyspnea was a focus of several studies. Chou et al. (2012) [38] examined sepsis-related respiratory failure in stage III and IV lung cancer patients, managing the condition with mechanical ventilation and transferring patients to long-term respiratory care if necessary. Cooksley et al. (2020) [39] addressed dyspnea related to immune checkpoint inhibitor toxicity, using steroids and antibiotics as interventions. In patients with advanced lung cancer, Kim et al. (2014) [50] identified multiple causes of dyspnea, such as obstructive pneumonia and chemo-induced lung toxicity, managed through vasoactive agents, hemodialysis, and mechanical ventilation. Additionally, Yilmaz et al. [77] explored the management of dyspnea in lung cancer patients with salbutamol and magnesium sulfate. Peyrony et al. (2021) [59] reported various supportive measures, including oxygen therapy and mechanical ventilation.
Addressing GI symptoms & bowel obstruction
GI symptoms included bowel obstruction, diarrhea, colitis, and nausea. Abelson et al. [29] and Frago et al. (2010) [43] both studied malignant large-bowel obstruction in colorectal cancer, which was treated with palliative stenting or chemotherapy regimens. Castillo et al. (2021) [36] focused on immune-related adverse events such as colitis and diarrhea, which were managed with corticosteroids including dexamethasone and prednisone. Teimouri et al. [68] also highlighted the use of steroids for managing GI toxicities, including colitis and hepatitis. In patients experiencing GI symptoms in the ED, Delgado-Guay et al. (2015) [41] noted the importance of palliative care consultations. Waddle et al. [71] reported on managing various GI symptoms and associated complications without specifying particular interventions.
Other treatment-related toxicities
Treatment-related toxicities are critical oncological emergencies, often requiring immediate intervention due to their potential severity and impact on patients' quality of life. Castillo et al. (2021) [36] explored immune-related adverse events (irAEs) such as colitis, diarrhea, hyperglycemia, and shortness of breath, managed with irAEs-specific treatments, primarily corticosteroids. Similarly, Teimouri et al. [68] focused on managing toxicities like diarrhea/colitis, hepatitis, pneumonitis, nephrotoxicity, and cardiotoxicity with steroids. In patients experiencing dyspnea, diarrhea, and fever related to treatment toxicity, Cooksley et al. (2020) [39] employed corticosteroids and antibiotics as treatment modalities.
Kim et al. (2014) [50] demonstrated a range of toxicities in lung cancer patients, including chemo-induced lung toxicity and radiation pneumonitis, addressing these conditions with interventions including vasoactive agents, hemodialysis, and mechanical ventilation. They emphasized that this comprehensive approach is vital to managing the acute and potentially life-threatening effects of cancer treatments. Xia and Wang (2016) [74] also reported on severe treatment-related toxicities in solid tumor patients, such as respiratory failure, septic shock, and acute renal failure, which necessitated the use of vasopressors, mechanical ventilation, and renal replacement therapy.
Lagman et al. [52] discussed the acute inpatient management of treatment-related complications, including neutropenic fever and radiation-induced pneumonitis, highlighting the use of various medications, invasive procedures, and supportive care measures to stabilize patients. Additionally, Abelson et al. [29] described interventions for malignant large-bowel obstruction secondary to colorectal cancer treatments, including palliative stenting or stoma creation.
Discussion
We conducted a systematic review of oncological emergencies and related interventions from 49 studies [29–77]. We examined the types and management of oncologic emergency-related ED visits and hospitalizations globally using data from multiple published sources. We observed that reports on oncological emergencies [4] varied widely, addressing infections with antibiotics and supportive care, pain with a range of analgesics, dyspnea with ventilatory support and other respiratory interventions, and GI symptoms with palliative procedures and steroid therapy. These interventions mitigate symptoms, improve quality of life, and reduce the impact on hospitalizations and ED visits worldwide.
Our findings are consistent with previous reports and similarly suggest that patients with cancer are at high risk for unplanned hospital use [78]. We expect ED use for oncologic emergencies to increase substantially in the next decade [79]. With over 63% of our identified articles reporting their total study population at an age over ≥ 60 years, we believe healthcare systems should prepare for an increase in patients requiring focused geriatric and supportive cancer care and management strategies in the ED. In accordance with this, we report that most interventions included lifesaving and often invasive procedures such as intubation, mechanical ventilation, and/or surgical procedures [29, 31, 34, 37, 38, 43, 46, 49, 50, 52, 57, 59, 63, 74]. Other prevalent interventions included steroids and/or antibiotics for infection [31, 34, 38–40, 42, 46, 57, 60–63, 65, 77]. and opioids for when patients presented with severe pain [32, 48, 52–54, 58, 59, 66, 72, 76]. With an expected increase in ED use by cancer patients, increased training for emergency department physicians may benefit the flow of oncological patients in the ED. Specifically, we recommend developing physician competency measures which ensures treating physicians are well equipped to provide symptom management and treatment related toxicity care. Although a majority of oncological emergencies presented in this review required an ED visit, further research is required to identify if we can minimize ED use by increasing access to management of emergencies in outpatient facilities.
Pain management remains a central concern in oncologic emergencies, with providers relying heavily on opioids, requiring patients and providers to mutually consider both the palliative benefits and associated risks of dependence and side effects. The use of various opioid formulations and adjunctive therapies such as acetaminophen and corticosteroids points to an ongoing need for optimizing pain control while minimizing adverse effects. Similarly, GI symptoms, including bowel obstruction, were frequently managed with palliative interventions such as stenting or specific chemotherapy regimens. The importance of specialized care, including palliative care consultations, reflected the complex nature of managing gastrointestinal complications during cancer treatment. The resources and time required in the ED to address these GI complications are limited; thus, challenges with exacerbations of complications are a primary concern.
The American Society of Clinical Oncology (ASCO) and National Cancer Institute (NCI) guidelines recommend early integration of palliative care as standard care alongside cancer care for patients with cancer. However, in many cases, palliative care is deferred until the EOL, with referrals often occurring in the last month of life (often in an inpatient setting) or not at all. Only one study [41] mentioned palliative care consultation in the ED and another study [70] reported EOL goals of care discussion. We found that pain is one of the most common reasons patients with cancer visit the ED; hence, providing palliative interventions to meet all their needs, including social and spiritual care, might be beneficial. Most importantly, studies focusing on patients admitted to acute inpatient palliative care units also reported administering invasive diagnostic and treatment procedures [52]. Most of the interventions reported as life-prolonging aggressive care suggest that there is a significant gap globally regarding the integration of palliative care in acute care settings.
This review indicates that while a broad array of treatments is available for managing oncologic emergencies, there is a lack of standardized protocols and guidelines, particularly for new cancer therapies such as immune checkpoint inhibitors. This variability in practice highlights the need for further research to develop evidence-based guidelines that can inform clinical decision-making and improve patient outcomes. A comprehensive, and integrative, approach will be crucial in improving the quality of care and outcomes for cancer patients facing emergencies.
Strengths and limitations
Our study identified diverse interventions used in the ED and other acute care settings for cancer-related concerns. We demonstrated a paramount need for palliative, hospice, and advanced care planning among this population. We have noted the need to strengthen endeavors that promote the integration of palliative care into standard emergency care for patients, especially those with cancer.
We restricted article inclusion to English language reviews and those reviews published in academic journals. Regarding the articles included, most studies did not report cancer type and treatment type, and we are unaware of the time required for intervention from these studies. Thus, we are unable to extrapolate the probability of emergent care according to the cancer type and complication. Most studies were conducted in a single site, which may limit the generalizability of findings due to variations in local healthcare practices, resources, and patient demographics. The heterogeneity in patient populations, with a significant proportion of studies not specifying cancer type, stage, or treatment, suggests a need for more granular data better to understand the specific needs of different patient subgroups.
Conclusions
Patients with cancer rely on the hospital for evaluation and management of disease and treatment-related concerns throughout their illnesses. However, studies reporting on oncologic emergencies are limited. These studies primarily focus on infection, pain, dyspnea, and GI symptoms with treatments including an array of interventions (e.g., opioids, invasive procedures). Most studies included older patients, suggesting that tailored interventions and management strategies are necessary to address the complex care needs (including social and palliative) of older patients with cancer. Further research may clarify the optimal management strategies to improve the outcomes for this vulnerable patient population.
Acknowledgements
The Comprehensive Oncologic Emergencies Research Network (CONCERN) supported this study with scientific review and suggestions on the study design and conduct.
Abbreviations
- APSCU
Acute Palliative-Supportive Care Unit
- ASCO
American Society of Clinical Oncology
- ASCT
Autologous Stem Cell Transplant
- BSI
Blood Stream Infection
- BTP
Breakthrough Pain
- CAR
Chimeric Antigen Receptor
- CAT
Cancer-associated Venous Thrombosis
- CED
Coverage with Evidence Development
- CPR
Cardiopulmonary Resuscitation
- CRC
Colorectal Cancer
- DVT
Deep Vein Thromboses
- ECG
Electrocardiogram
- ED
Emergency department
- EM
Emergency Medicine
- EOL
End of Life
- HM
Hematemesis and Melena
- HDT
High-dose Therapy
- HSCT
Hematopoietic Stem Cell Transplant
- ICD-9
International Classification of Diseases V9th Rev
- ICI
Immune Checkpoint Inhibitors
- ICU
Intensive Care Unit
- INF
Intranasal Fentanyl
- irAEs
Immune-related Adverse Events
- IV
Intravenous
- IVH
Intravenous Hydromorphone
- GI
Gastrointestinal
- KAMC
HC – King Abdullah Medical Health Clusters
- NCI
National Cancer Institute
- NEDI
National Emergency Department Inventories
- NRS
Numeric Rating Scale
- PE
Pulmonary Embolism
- PRESS
Peer Review of Electronic Search Strategies
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
Randomized Controlled Trial
- TLS
Tumor lysis Syndrome
- UTI
Urinary Tract Infection
- VRE
Vancomycin-Resistant Enterococcus
- VTE
Venous Thromboembolism
Authors’ contributions
All authors made substantial contribution to the study including but not limited to the conception, design, data collection and interpretation and review and editing. SY, KA, JK, JJB, ASH, NW, BEGR, MFH, SWH, MKW, CJC, and CRG: took lead in the conception and design, original draft, data interpretation, review and editing.
Funding
T32CA102618 (Yilmaz), American Cancer Society CSDG-20–023-01-CPHPS (Hong).
Data availability
The dataset used and/or analyzed during the current study is available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Bonnie E. Gould Rothberg: Stock Ownership: Butterfly Networks Inc., Quantum Si, Hyperfine Research, AI Therapeutics, Detect Labs, identifeye Health, Protein Evolution Inc.) and direct family members: #A) Stock Ownership: Butterfly Networks Inc., Quantum Si, Hyperfine Research, AI Therapeutics, Detect Labs, identifeye Health, Protein Evolution Inc., 454 Corporation, Electric Futures, (Abbvie Inc, Amgen inc, Biocryst Pharmaceuticals, Gilead Sciences, Inc, Regeneron Pharmaceuticals Inc, Roche Holdings, Pacific Biosciences of California Inc (sold 07/2023)), Telesis Bio Inc #B) Employment: Butterfly Networks Inc, 4Catalyzer #C) Significant Leadership: Butterfly Networks Inc, Quantum Si, Hyperfine Research, AI Therapeutics, identifyee Health, Detect Labs, Protein Evolution Inc. #D) Patents, Royalties, and Other Intellectual Property: Thermo Fisher, Butterfly Networks, Quantum Si, Hyperfine Research, AI Therapeutics, Tesseract, Detect Labs. Christopher William Baugh: paid speaker for Roche Diagnostics, Octapharma, and CE Symmetry, an investigator for Abbott Laboratories, an advisory board participant for Roche Diagnostics, Salix Pharmaceuticals, Pfizer Inc., and AstraZeneca, a consultant for Abbott, Pfizer, Roche, and an advisor to Lucia Health Guidelines. Sai-Ching Yeung: an advisory board participant Salix Pharmaceuticals. The remaining authors declare that they have no competing interests.
Christopher William Baugh: paid speaker for Roche Diagnostics, Octapharma, and CE Symmetry, an investigator for Abbott Laboratories, an advisory board participant for Roche Diagnostics, Salix Pharmaceuticals, Pfizer Inc., and AstraZeneca, a consultant for Abbott, Pfizer, Roche, and an advisor to Lucia Health Guidelines.
Sai-Ching Yeung: an advisory board participant Salix Pharmaceuticals.
The remaining authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sule Yilmaz and Komal Aryal Co-first authors.
References
- 1.Al Nuhait M, Bajnaid E, Al Otaibi A, Al Shammari A, Al AY. Real-world safety experience with immune checkpoint inhibitors in Saudi Arabia. Sci Prog. 2021;104(1):36850421997302. 10.1177/0036850421997302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Isikber C, Gulen M, Satar S, Avci A, Acehan S, Isikber GG, Yesiloglu O. Evaluation of the frequency of patients with cancer presenting to an emergency department. Rev Assoc Med Bras (1992). 2020;66(10):1402–8. 10.1590/1806-9282.66.10.1402. [DOI] [PubMed] [Google Scholar]
- 3.Panattoni L, Fedorenko C, Greenwood-Hickman MA, et al. Characterizing Potentially Preventable Cancer- and Chronic Disease-Related Emergency Department Use in the Year After Treatment Initiation: A Regional Study. J Oncol Pract. 2018;14(3):e176–85. 10.1200/jop.2017.028191. [DOI] [PubMed] [Google Scholar]
- 4.Gould Rothberg B, Quest T, Yeung SC, et al. Oncologic emergencies and urgencies: A comprehensive review. CA: Cancer J Clin. 2022;72(6):570–93. 10.3322/caac.21727. [DOI] [PubMed] [Google Scholar]
- 5.Sadik M, Ozlem K, Huseyin M, AliAyberk B, Ahmet S, Ozgur O. Attributes of cancer patients admitted to the emergency department in one year. World J Emerg Med. 2014;5(2):85–90. 10.5847/wjem.j.issn.1920-8642.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alishahi Tabriz A, Turner K, Hong YR, Gheytasvand S, Powers BD, Elston Lafata J. Trends and Characteristics of Potentially Preventable Emergency Department Visits Among Patients With Cancer in the US. JAMA Netw Open. 2023;6(1):e2250423. 10.1001/jamanetworkopen.2022.50423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rivera DR, Gallicchio L, Brown J, Liu B, Kyriacou DN, Shelburne N. Trends in Adult Cancer-Related Emergency Department Utilization: An Analysis of Data From the Nationwide Emergency Department Sample. JAMA Oncol. 2017;3(10):e172450. 10.1001/jamaoncol.2017.2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adler D, Abar B, Durham DD, et al. Validation of the Emergency Severity Index (Version 4) for the Triage of Adult Emergency Department Patients With Active Cancer. J Emerg Med. 2019;57(3):354–61. 10.1016/j.jemermed.2019.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lash RS, Hong AS, Bell JF, Reed SC, Pettit N. Recognizing the emergency department’s role in oncologic care: a review of the literature on unplanned acute care. Emerg Cancer Care. 2022;1(1):6. 10.1186/s44201-022-00007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen H, Walabyeki J, Johnson M, Boland E, Seymour J, Macleod U. An integrated understanding of the complex drivers of emergency presentations and admissions in cancer patients: Qualitative modelling of secondary-care health professionals’ experiences and views. PLoS ONE. 2019;14(5): e0216430. 10.1371/journal.pone.0216430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dumnui N, Nagaviroj K, Anothaisintawee T. A study of the factors associated with emergency department visits in advanced cancer patients receiving palliative care. BMC Palliative Care. 2022;21(1):197. 10.1186/s12904-022-01098-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gallaway MS, Idaikkadar N, Tai E, et al. Emergency department visits among people with cancer: Frequency, symptoms, and characteristics. J Am Coll Emerg Physicians Open. 2021;2(3). 10.1002/emp2.12438. [DOI] [PMC free article] [PubMed]
- 13.Rico JF, Caterino JM, Stephens JA, et al. Variables associated with admission rates among cancer patients presenting to emergency departments: a CONCERN group study. Emerg Cancer Care. 2023;2(1):7. 10.1186/s44201-023-00022-z. [Google Scholar]
- 14.Mayer DK, Travers D, Wyss A, Leak A, Waller A. Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol. 2011;29(19):2683–8. 10.1200/jco.2010.34.2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vandyk AD, Harrison MB, Macartney G, Ross-White A, Stacey D. Emergency department visits for symptoms experienced by oncology patients: a systematic review. Support Care Cancer. 2012;20(8):1589–99. 10.1007/s00520-012-1459-y. [DOI] [PubMed] [Google Scholar]
- 16.Schuur JD, Venkatesh AK. The growing role of emergency departments in hospital admissions. N Engl J Med. 2012;367(5):391–3. 10.1056/NEJMp1204431. [DOI] [PubMed] [Google Scholar]
- 17.Fleshner L, Lagree A, Shiner A, et al. Drivers of Emergency Department Use Among Oncology Patients in the Era of Novel Cancer Therapeutics: A Systematic Review. Oncologist. 2023;28(12):1020–33. 10.1093/oncolo/oyad161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCaig L, Xu, J., & Niska, R. Estimates of Emergency Department Capacity: United States, 2007. Centers for Disease Control and Prevention. 2015. https://www.cdc.gov/nchs/data/hestat/ed_capacity/ed_capacity.htm.
- 19.Steptoe AP, Corel B, Sullivan AF, Camargo CA. Characterizing emergency departments to improve understanding of emergency care systems. Int J Emerg Med. 2011;4(1):42. 10.1186/1865-1380-4-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wen LS, Xu J, Steptoe AP, Sullivan AF, Walline JH, Yu X, Camargo CA Jr. Emergency department characteristics and capabilities in Beijing. China J Emerg Med. 2013;44(6):1174-1179.e4. 10.1016/j.jemermed.2012.07.083. [DOI] [PubMed] [Google Scholar]
- 21.Maldonado A, Patiño AM, Kearney AS, et al. Emergency Department Characteristics and Capabilities in Quito, Ecuador. Ann Glob Health. 2021;87(1):37. 10.5334/aogh.3129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jaklic B, Wen L, Sullivan A, Camargo C. A Profile of Emergency Departments in Slovenia. ISRN Emergency Medicine; 2012. 10.5402/2012/461274.
- 23.Naouri D, El Khoury C, Vincent-Cassy C, Vuagnat A, Schmidt J, Yordanov Y. The French Emergency National Survey: A description of emergency departments and patients in France. PLoS ONE. 2018;13(6): e0198474. 10.1371/journal.pone.0198474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wen LS, Oshiomogho JI, Eluwa GI, Steptoe AP, Sullivan AF, Camargo CA Jr. Characteristics and capabilities of emergency departments in Abuja. Nigeria Emerg Med J. 2012;29(10):798–801. 10.1136/emermed-2011-200695. [DOI] [PubMed] [Google Scholar]
- 25.van der Meer DM, Weiland TJ, Philip J, et al. Presentation patterns and outcomes of patients with cancer accessing care in emergency departments in Victoria Australia. Support Care Cancer. 2016;24(3):1251–60. 10.1007/s00520-015-2921-4. [DOI] [PubMed] [Google Scholar]
- 26.Hsu J, Donnelly JP, Moore JX, Meneses K, Williams G, Wang HE. National characteristics of Emergency Department visits by patients with cancer in the United States. Am J Emerg Med. 2018;36(11):2038–43. 10.1016/j.ajem.2018.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Min HS, Chang HJ, Sung HK. Emergency Department Utilization of Adult Cancer Patient in Korea: A Nationwide Population-Based Study, 2017–2019. Cancer Res Treat. 2022;54(3):680–9. 10.4143/crt.2021.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. 2021;372:n71. 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abelson JS, Yeo HL, Mao J, Milsom JW, Sedrakyan A. Long-term Postprocedural Outcomes of Palliative Emergency Stenting vs Stoma in Malignant Large-Bowel Obstruction. JAMA Surg. 2017;152(5):429–35. 10.1001/jamasurg.2016.5043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alsirafy SA, Raheem AA, Al-Zahrani AS, Mohammed AA, Sherisher MA, El-Kashif AT, Ghanem HM. Emergency Department Visits at the End of Life of Patients With Terminal Cancer: Pattern, Causes, and Avoidability. Am J Hosp Palliat Care. 2016;33(7):658–62. 10.1177/1049909115581819. [DOI] [PubMed] [Google Scholar]
- 31.Azoulay É, Castro P, Maamar A, et al. Outcomes in patients treated with chimeric antigen receptor T-cell therapy who were admitted to intensive care (CARTTAS): an international, multicentre, observational cohort study. Lancet Haematol. 2021;8(5):e355–64. 10.1016/s2352-3026(21)00060-0. [DOI] [PubMed] [Google Scholar]
- 32.Banala SR, Khattab OK, Page VD, Warneke CL, Todd KH, Yeung SJ. Intranasal fentanyl spray versus intravenous opioids for the treatment of severe pain in patients with cancer in the emergency department setting: A randomized controlled trial. PLoS ONE. 2020;15(7): e0235461. 10.1371/journal.pone.0235461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bosscher MR, Bastiaannet E, van Leeuwen BL, Hoekstra HJ. Factors Associated with Short-Term Mortality After Surgical Oncologic Emergencies. Ann Surg Oncol. 2016;23(6):1803–14. 10.1245/s10434-015-4939-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bou Chebl R, Safa R, Sabra M, et al. Sepsis in patients with haematological versus solid cancer: a retrospective cohort study. BMJ Open. 2021;11(2):e038349. 10.1136/bmjopen-2020-038349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bow EJ, Rotstein C, Noskin GA, et al. A randomized, open-label, multicenter comparative study of the efficacy and safety of piperacillin-tazobactam and cefepime for the empirical treatment of febrile neutropenic episodes in patients with hematologic malignancies. Clin Infect Dis. 2006;43(4):447–59. 10.1086/505393. [DOI] [PubMed] [Google Scholar]
- 36.Castillo RM, Sandefur BJ, Finch AS, Richter MD, Thanarajasingam U. Clinical Presentations and Outcomes of Patients Receiving Immune Checkpoint Inhibitors Presenting to the Emergency Department. Mayo Clin Proc Innov Qual Outcomes. 2021;5(6):1029–35. 10.1016/j.mayocpiqo.2021.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cauley CE, Panizales MT, Reznor G, et al. Outcomes after emergency abdominal surgery in patients with advanced cancer: Opportunities to reduce complications and improve palliative care. J Trauma Acute Care Surg. 2015;79(3):399–406. 10.1097/ta.0000000000000764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chou KT, Chen CS, Su KC, et al. Hospital outcomes for patients with stage III and IV lung cancer admitted to the intensive care unit for sepsis-related acute respiratory failure. J Palliat Med. 2012;15(11):1234–9. 10.1089/jpm.2012.0084. [DOI] [PubMed] [Google Scholar]
- 39.Cooksley T, Gupta A, Al-Sayed T, Lorigan P. Emergency presentations in patients treated with immune checkpoint inhibitors. Eur J Cancer. 2020;130:193–7. 10.1016/j.ejca.2020.02.025. [DOI] [PubMed] [Google Scholar]
- 40.Coyne CJ, Reyes-Gibby CC, Durham DD, et al. Cancer pain management in the emergency department: a multicenter prospective observational trial of the Comprehensive Oncologic Emergencies Research Network (CONCERN). Support Care Cancer. 2021;29(8):4543–53. 10.1007/s00520-021-05987-3. [DOI] [PubMed] [Google Scholar]
- 41.Delgado-Guay MO, Kim YJ, Shin SH, Chisholm G, Williams J, Allo J, Bruera E. Avoidable and unavoidable visits to the emergency department among patients with advanced cancer receiving outpatient palliative care. J Pain Symptom Manage. 2015;49(3):497–504. 10.1016/j.jpainsymman.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 42.De Silva N, Jackson J, Steer C. Infections, resistance patterns and antibiotic use in patients at a regional cancer centre. Intern Med J. 2018;48(3):323–9. 10.1111/imj.13646. [DOI] [PubMed] [Google Scholar]
- 43.Frago R, Kreisler E, Biondo S, Salazar R, Dominguez J, Escalante E. Outcomes in the management of obstructive unresectable stage IV colorectal cancer. Eur J Surg Oncol. 2010;36(12):1187–94. 10.1016/j.ejso.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 44.Giustozzi M, Connors JM, Ruperez Blanco AB, et al. Clinical characteristics and outcomes of incidental venous thromboembolism in cancer patients: Insights from the Caravaggio study. J Thromb Haemost. 2021;19(11):2751–9. 10.1111/jth.15461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grewal K, Krzyzanowska MK, McLeod S, Borgundvaag B, Atzema CL. Outcomes after emergency department use in patients with cancer receiving chemotherapy in Ontario, Canada: a population-based cohort study. CMAJ Open. 2020;8(3):E496-e505. 10.9778/cmajo.20190198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gudiol C, Royo-Cebrecos C, Laporte J, et al. Clinical features, aetiology and outcome of bacteraemic pneumonia in neutropenic cancer patients. Respirology. 2016;21(8):1411–8. 10.1111/resp.12848. [DOI] [PubMed] [Google Scholar]
- 47.Hsu HS, Wu TH, Lin CY, Lin CC, Chen TP, Lin WY. Enhanced home palliative care could reduce emergency department visits due to non-organic dyspnea among cancer patients: a retrospective cohort study. BMC Palliat Care. 2021;20(1):42. 10.1186/s12904-021-00713-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kao YH, Liu YT, Koo M, Chiang JK. Factors associated with emergency services use in Taiwanese advanced cancer patients receiving palliative home care services during out-of-hours periods: a retrospective medical record study. BMC Palliat Care. 2018;17(1):46. 10.1186/s12904-018-0302-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kerhuel L, Amorim S, Azoulay E, Thiéblemont C, Canet E. Clinical features of life-threatening complications following autologous stem cell transplantation in patients with lymphoma. Leuk Lymphoma. 2015;56(11):3090–5. 10.3109/10428194.2015.1034700. [DOI] [PubMed] [Google Scholar]
- 50.Kim YJ, Kim MJ, Cho YJ, et al. Who should be admitted to the intensive care unit? The outcome of intensive care unit admission in stage IIIB-IV lung cancer patients. Med Oncol. 2014;31(3):847. 10.1007/s12032-014-0847-1. [DOI] [PubMed] [Google Scholar]
- 51.Klamroth R, Sinn M, Pollich C, et al. Anticoagulation Practice in Patients with Cancer-Associated Thrombosis: Insights from GeCAT, a German Prospective Registry Study. Oncol Res Treat. 2022;45(4):178–85. 10.1159/000521698. [DOI] [PubMed] [Google Scholar]
- 52.Lagman R, Rivera N, Walsh D, LeGrand S, Davis MP. Acute inpatient palliative medicine in a cancer center: clinical problems and medical interventions–a prospective study. Am J Hosp Palliat Care. 2007;24(1):20–8. 10.1177/1049909106295292. [DOI] [PubMed] [Google Scholar]
- 53.Mercadante S, Villari P, Ferrera P, Mangione S, Casuccio A. The use of opioids for breakthrough pain in acute palliative care unit by using doses proportional to opioid basal regimen. Clin J Pain. 2010;26(4):306–9. 10.1097/AJP.0b013e3181c4458a. [DOI] [PubMed] [Google Scholar]
- 54.Mercadante S, Adile C, Ferrera P, Casuccio A. Characteristics of advanced cancer patients who were readmitted to an acute palliative/supportive care unit. Support Care Cancer. 2017;25(6):1947–52. 10.1007/s00520-017-3604-0. [DOI] [PubMed] [Google Scholar]
- 55.Miranda B, Vidal SA, Mello MJ, et al. Cancer patients, emergencies service and provision of palliative care. Rev Assoc Med Bras (1992). 2016;62(3):207–11. 10.1590/1806-9282.62.03.207. [DOI] [PubMed] [Google Scholar]
- 56.Moghnieh R, Estaitieh N, Mugharbil A, et al. Third generation cephalosporin resistant Enterobacteriaceae and multidrug resistant gram-negative bacteria causing bacteremia in febrile neutropenia adult cancer patients in Lebanon, broad spectrum antibiotics use as a major risk factor, and correlation with poor prognosis. Front Cell Infect Microbiol. 2015;5:11. 10.3389/fcimb.2015.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Numico G, Cristofano A, Mozzicafreddo A, et al. Hospital admission of cancer patients: avoidable practice or necessary care? PLoS ONE. 2015;10(3): e0120827. 10.1371/journal.pone.0120827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Patel PM, Goodman LF, Knepel SA, et al. Evaluation of Emergency Department Management of Opioid-Tolerant Cancer Patients With Acute Pain. J Pain Symptom Manage. 2017;54(4):501–7. 10.1016/j.jpainsymman.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 59.Peyrony O, Fontaine JP, Trabattoni E, et al. Cancer Patients' Prehospital Emergency Care: Post Hoc Analysis from the French Prospective Multicenter Study EPICANCER. J Clin Med. 2021;10(5) 10.3390/jcm10051145. [DOI] [PMC free article] [PubMed]
- 60.Poutsiaka DD, Skiffington S, Miller KB, Hadley S, Snydman DR. Daptomycin in the treatment of vancomycin-resistant Enterococcus faecium bacteremia in neutropenic patients. J Infect. 2007;54(6):567–71. 10.1016/j.jinf.2006.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Raghavendra M, Hoeg RT, Bottner WA, Agger WA. Management of neutropenic fever during a transition from traditional hematology/oncology service to hospitalist care. WMJ. 2014;113(2):53–8. [PubMed] [Google Scholar]
- 62.Rolston KV, Frisbee-Hume SE, Patel S, Manzullo EF, Benjamin RS. Oral moxifloxacin for outpatient treatment of low-risk, febrile neutropenic patients. Support Care Cancer. 2010;18(1):89–94. 10.1007/s00520-009-0634-2. [DOI] [PubMed] [Google Scholar]
- 63.Ruiz-Artacho P, Trujillo-Santos J, López-Jiménez L, et al. Clinical Characteristics and Outcomes of Patients with Lung Cancer and Venous Thromboembolism. TH Open. 2018;2(2):e210–7. 10.1055/s-0038-1656542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sandgren A, Fridlund B, Nyberg P, Strang P, Petersson K, Thulesius H. Symptoms, care needs and diagnosis in palliative cancer patients in acute care hospitals: a 5-year follow-up survey. Acta Oncol. 2010;49(4):460–6. 10.3109/02841860903463991. [DOI] [PubMed] [Google Scholar]
- 65.Skiba R, Sikotra N, Ball T, Arellano A, Gabbay E, Clay TD. Management of neutropenic fever in a private hospital oncology unit. Intern Med J. 2020;50(8):959–64. 10.1111/imj.14464. [DOI] [PubMed] [Google Scholar]
- 66.Soares LG, Martins M, Uchoa R. Intravenous fentanyl for cancer pain: a “fast titration” protocol for the emergency room. J Pain Symptom Manage. 2003;26(3):876–81. 10.1016/s0885-3924(03)00314-2. [DOI] [PubMed] [Google Scholar]
- 67.Sutradhar R, Barbera L, Seow HY. Palliative homecare is associated with reduced high- and low-acuity emergency department visits at the end of life: A population-based cohort study of cancer decedents. Palliat Med. 2017;31(5):448–55. 10.1177/0269216316663508. [DOI] [PubMed] [Google Scholar]
- 68.Teimouri A, Minard LV, Scott SN, Daniels A, Snow S. Real-World Adherence to Toxicity Management Guidelines for Immune-Related Adverse Events. Curr Oncol. 2022;29(5):3104–17. 10.3390/curroncol29050252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Verhoef MJ, de Nijs E, Horeweg N, et al. Palliative care needs of advanced cancer patients in the emergency department at the end of life: an observational cohort study. Support Care Cancer. 2020;28(3):1097–107. 10.1007/s00520-019-04906-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Verhoef MJ, de Nijs EJM, Ootjers CS, et al. End-of-Life Trajectories of Patients With Hematological Malignancies and Patients With Advanced Solid Tumors Visiting the Emergency Department: The Need for a Proactive Integrated Care Approach. Am J Hosp Palliat Care. 2020;37(9):692–700. 10.1177/1049909119896533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Waddle MR, Chen RC, Arastu NH, et al. Unanticipated hospital admissions during or soon after radiation therapy: Incidence and predictive factors. Pract Radiat Oncol. 2015;5(3):e245–53. 10.1016/j.prro.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 72.Won YH, Choi YJ, Ahn S, et al. Improving the quality of cancer pain management in an academic medical center emergency department. Clin J Oncol Nurs. 2014;18(6):626–9. 10.1188/14.Cjon.626-629. [DOI] [PubMed] [Google Scholar]
- 73.Woon DTS, Finelli A, Cheung DC, et al. A Population-based Study Comparing Outcomes for Patients With Metastatic Castrate Resistant Prostate Cancer Treated by Urologists or Medical Oncologists With First Line Abiraterone Acetate or Enzalutamide. Urology. 2021;153:147–55. 10.1016/j.urology.2020.11.080. [DOI] [PubMed] [Google Scholar]
- 74.Xia R, Wang D. Intensive care unit prognostic factors in critically ill patients with advanced solid tumors: a 3-year retrospective study. BMC Cancer. 2016;16:188. 10.1186/s12885-016-2242-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yaman S, Başcı S, Turan G, et al. Single-Dose Rasburicase Might Be Adequate To Overcome Tumor Lysis Syndrome In Hematological Malignancies. Clin Lymphoma Myeloma Leuk. 2022;22(2):e71–6. 10.1016/j.clml.2021.08.009. [DOI] [PubMed] [Google Scholar]
- 76.Yildirim B, Tanriverdi O. Evaluation of cancer patients admitted to the emergency department within one month before death in Turkey: what are the problems needing attention? Asian Pac J Cancer Prev. 2014;15(1):349–53. 10.7314/apjcp.2014.15.1.349. [DOI] [PubMed] [Google Scholar]
- 77.Yilmaz SYE, Yuksel M, et al. Nonopioid therapy for cancer related dyspnea palliation in the ED: A randomized double blind clinical trial. Acta Medica Mediterranea. 2017;6:1099–106. [Google Scholar]
- 78.Shen J, Xing Q, Xu Q, Qian J. Cancer patients in the emergency department or intensive care unit: a 20-year bibliometric analysis of research progress and prospects. Emerg Cancer Care. 2023;2(1):5. [Google Scholar]
- 79.Liebregts T, Lueck C, Mohring A, Riße J, Tzalavras A. Cancer patients in the emergency department. Med Klin Intensivmed Notfmed. 2024;119(1):3–9. 10.1007/s00063-023-01055-2. Krebspatienten in der Notaufnahme. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset used and/or analyzed during the current study is available from the corresponding author upon reasonable request.