Abstract
Background:
In early 2015, a patient from a cluster of cases of Ebola Virus Disease (EVD) in Monrovia, Liberia traveled to a rural village in Margibi County, potentially exposing numerous persons. The patient died in the village and post-mortem testing confirmed Ebola Virus infection.
Problem:
The Margibi County Health Team (CHT; Kakata, Margibi, Liberia) needed to prevent further transmission of EVD within and outside of the affected villages, and they needed to better understand the factors that support or impede compliance with measures to stop the spread of EVD.
Methods:
In February-March 2015, the Margibi CHT instituted a 21-day quarantine and active monitoring for two villages where the patient had contact with numerous residents, and a 21-day active monitoring for five other villages where the patient had possible contact with an unknown number of persons. One contact developed EVD and quarantine was extended an additional 12 days in one village. In April 2015, the Margibi CHT conducted a household-based EVD knowledge, attitudes, and practices (KAP) survey of the seven villages. From April 24–29, 2015, interview teams approached every household in the seven villages and collected information on demographics, knowledge of EVD, attitudes about quarantine to prevent the spread of EVD, and their quarantine experiences and practices. Descriptive statistics were calculated.
Results:
One hundred fifteen interviews were conducted, representing the majority of the households in the seven villages. Most (99%) correctly identified touching an infected person’s body fluids and contact with the body of someone who has died from EVD as transmission routes. However, interviewees sometimes incorrectly identified mosquito bites (58%) and airborne spread (32%) as routes of EVD transmission, and 72% incorrectly identified the longest EVD incubation period as ≤ seven days. Eight of 16 households in the two quarantined villages (50%) reported times when there was not enough water or food during quarantine. Nine of 16 (56%) reported that a household member had illnesses or injuries during quarantine; of these, all (100%) obtained care from a clinic, hospital, or Ebola treatment unit (ETU).
Conclusion:
Residents’ knowledge of EVD transmission routes and incubation period were suboptimal. Public health authorities should consider assessing residents’ understanding of Ebola transmission routes and effectively educate them to ensure correct understanding. Quarantined residents should be provided with sufficient food, water, and access to medical care.
Keywords: Ebola Virus Disease, quarantine, transmission
Introduction
In early 2015, a cluster of 22 cases of Ebola Virus Disease (EVD) in Monrovia, Liberia was identified and contained after three generations of transmission.1 A patient from this cluster (Patient A, 2nd generation of EVD transmission) became ill on January 27 and travelled using a different name to a rural village (Village A) in Margibi County (Figure 1). He was cared for by family in Village A, had contact with numerous people in Village A and nearby Village B, and had possible contact with an unknown number of persons in five other nearby villages (Villages C-G). He died on February 1 in Village A and was safely buried on February 2. Post-mortem testing of an oral swab collected on February 2 confirmed Ebola Virus infection, prompting the Margibi County Health Team (CHT; Kakata, Margibi, Liberia) to initiate active monitoring for all residents of Villages A-G and community quarantine for Villages A and B from February 3–23.
Figure 1.
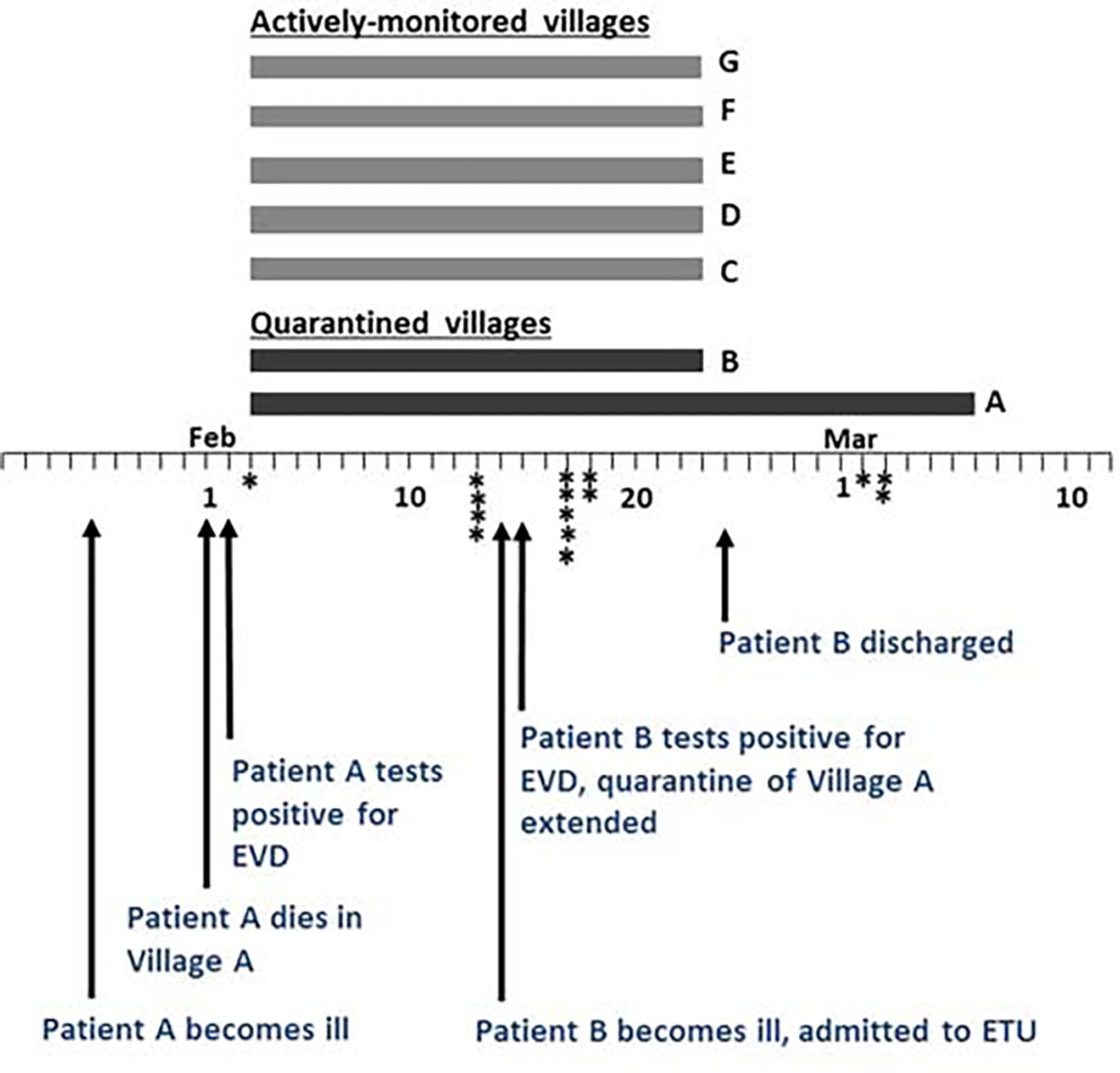
Timeline of Events Surrounding the Active Monitoring and Quarantine of Seven Rural Villages, Margibi County, Liberia, January-March 2015.
Note: Duration of quarantine of Villages A and B and active monitoring of Villages C-G are represented by bars. Asterisks indicate date at which a resident in Village A or B was admitted to the ETU with illness later determined to be non-EVD.
Abbreviations: ETU, Ebola treatment unit; EVD, Ebola Virus Disease.
Methods
Outbreak Response
The Margibi CHT met with Town Chiefs and households of each village to initiate and sustain active monitoring and quarantine. Residents of quarantined villages were restricted from leaving their village, including for going to work, school, or market. The CHT contact tracers and case finders were instructed to visit all residents of each village twice daily and screen them for signs and symptoms of EVD. The CHT and emergency partners coordinated delivery of food and water to quarantined villages.
On February 14, case finders identified a Village A resident with EVD-consistent illness. She was transported to the Margibi Ebola treatment unit (ETU), and on February 15, tested positive for Ebola Virus infection (Patient B, 3rd generation of EVD transmission). The Margibi CHT extended the quarantine of Village A until March 7. Patient B recovered at the ETU and was discharged on February 24; the Margibi CHT held a reintegration ceremony for Patient B at Village A the same day (Figure 2).
Figure 2.

In-Person Interactions between Margibi County Health Team and Actively Monitored or Quarantined Villages.
Panel A. Re-integration ceremony for Patient A at Village A. The Margibi County Health Officer explains to Village A residents that Patient A is Ebola-free and should be welcomed back into her community as an ambassador in the fight against Ebola (February 24, 2015).
Panel B. The Margibi CHT explains to a village that their active monitoring period is complete, but that they should refrain from entering Village A until Village A’s quarantine period is complete.
During the 33-day and 20-day quarantines of Villages A and B, respectively, case finders identified an additional 15 persons with suspected EVD (Figure 1). Each was transported to the Margibi ETU and tested for EVD infection twice over a 3-day period. None tested positive. On February 23 and March 7, the Margibi CHT lifted the quarantine or monitoring at Villages B-G and A, respectively (Figure 2).
Knowledge, Attitudes, and Practices Survey
Though community quarantines have been implemented to control EVD transmission,2–6 no reports have described factors that supported compliance or led to barriers complying with quarantine restrictions. A head-of-household knowledge, attitudes, and practices (KAP) questionnaire that included questions about EVD; attitudes about quarantine to prevent the spread of EVD; and for Villages A and B, experiences and practices during quarantine was designed by the Centers for Disease Control and Prevention (CDC; Atlanta, Georgia USA), the CHT, and Peace Corps staff (Appendix 1; available online only). Two Liberian Peace Corps staff compared their interpretation of each survey question and constructed Liberian English versions of each question by consensus. Liberian English questions were used when preferred by interviewed households. Every household in Villages A-G was approached April 24–29 by local YMCA volunteers trained by Liberian Peace Corps staff. The Human Subjects Research Office of the CDC approved this assessment as public health practice (public health emergency response and program evaluation; Human Subjects Review #EOC Ebola Response 2015 1017) and the assessment was approved by the Margibi County Health Officer.
Results
Teams completed seven, nine, and 99 interviews in Villages A, B, and C-G, respectively. The Margibi CHT previously had estimated the population of Villages A, C, F, and G as 71, 96, 67, and 55, respectively, but had no estimates for number of households, and also did not have population estimates for Villages B, D, or E. The sum of persons living in interviewed households in Villages A, C, F, and G was 56, 95, 42, and 39, respectively; therefore, similar representation was estimated by interviewed households for the population of these villages (80%), quarantined villages (79%), and 81% of the total population of these villages was likely represented by interviewed households of monitored villages.
Respondents correctly identified vomiting (96%), diarrhea/“running stomach” (88%), red eyes (80%), fever/“hot skin” (64%), and weakness (62%) as signs and symptoms of EVD (Table 1). Most (99%) correctly identified contact with an infected person’s bodily fluids or with the body of someone who had died from EVD as routes of transmission, but mosquito bites and airborne/“through the air like a fresh cold” were incorrectly identified by 58% and 32%, respectively. Although most (74%) correctly identified that EVD could be caught from an infected person only after they showed signs of illness, most (72%) incorrectly identified the longest number of days after catching Ebola before a person becomes sick as ≤ seven. These data indicate that residents were well-informed about the signs and symptoms of EVD, but that knowledge of EVD transmission routes and incubation period (and likely the rationale for a 21-day monitoring/quarantine period) was suboptimal.
Table 1.
Knowledge of EVD and Attitudes about Community Quarantine, Villages A-G (N = 115), Margibi County, Liberia
| All Villages (n = 115) | Villages A and B (n = 16) | Villages C-G (n = 99) | |
|---|---|---|---|
| Knowledge about Ebola: | No. (%) | ||
| What are the signs and symptoms of Ebola?a | |||
| Vomiting | 110 (96) | 16 (100) | 94 (95) |
| Diarrhea (running stomach) | 101 (88) | 12 (75) | 89 (90) |
| Red Eyes | 92 (80) | 14 (88) | 78 (79) |
| Fever (hot skin) | 74 (64) | 8 (50) | 66 (67) |
| Weakness | 71 (62) | 10 (63) | 61 (62) |
| Bleeding | 43 (37) | 9 (56) | 34 (34) |
| Bleeding Gums | 6 (5) | 2 (13) | 4 (4) |
| Headache | 5 (4) | 1 (6) | 4 (4) |
| Hiccups | 5 (4) | 1 (6) | 4 (4) |
| How does Ebola spread? | |||
| Touching an infected person’s body fluids | 114 (99) | 16 (100) | 98 (99) |
| Contact with the body of someone who has died from Ebola | 114 (99) | 16 (100) | 98 (99) |
| Drinking water in the same town as someone who has Ebola | 108 (94) | 14 (88) | 94 (95) |
| Mosquito bites | 67 (58) | 11 (69) | 56 (57) |
| Airborne (through the air like a fresh cold) | 37 (32) | 6 (38) | 31 (31) |
| When can a person catch Ebola from an infected person? | |||
| Before they show signs of Ebola illness | 26 (23) | 6 (38) | 20 (20) |
| After they show signs of Ebola illness | 85 (74) | 9 (56) | 76 (77) |
| After they survive Ebola illness | 2 (2) | 0 (0) | 2 (2) |
| After they have negative test after surviving Ebola illness | 2 (2) | 1 (6) | 1 (1) |
| What is the longest number of days after catching Ebola before a person becomes sick?b | |||
| 0 | 30 (26) | 5 (31) | 25 (25) |
| 1–7 | 53 (46) | 7 (42) | 46 (46) |
| 8–20 | 8 (7) | 2 (13) | 6 (6) |
| 21 | 24 (21) | 2 (13) | 22 (22) |
| Attitudes about Quarantine: c | |||
| Quarantine can slow the spread of Ebola | 106 (92) | 14 (88) | 92 (93) |
| Anyone who is told to stay in quarantine is at risk for Ebola | 41 (36) | 10 (63) | 31 (31) |
| Quarantine means staying inside a quarantined area | 112 (97) | 16 (100) | 96 (97) |
| A person who is told they live in a quarantined area should stay there until they’re told they can go | 115 (100) | 16 (100) | 99 (100) |
| A person who leaves a quarantined area before they are told they can leave may become ill with Ebola and others may catch it from them | 111 (97) | 15 (94) | 96 (97) |
| Staying in quarantine does protect my family | 113 (98) | 16 (100) | 97 (98) |
| Quarantine is good for my family and friends | 108 (94) | 13 (81) | 95 (96) |
| A person in a quarantined area deserves to have adequate water, food, and other basic needs including going to clinics if they become ill | 115 (100) | 16 (100) | 99 (100) |
| If you were in a quarantine area you would stay there until the County Health Team said you could go outside | 114 (99) | 16 (100) | 98 (99) |
| I would follow my Town Chief’s directions about quarantine | 113 (98) | 16 (100) | 97 (98) |
| I would follow the County Health Team’s directions about quarantine | 115 (100) | 16 (100) | 99 (100) |
| I would tell others in my village to stay inside quarantine area if they said they were going to leave or were going to ignore Town Chief or County Health directions | 114 (99) | 15 (94) | 99 (100) |
Abbreviation: EVD, Ebola Virus Disease.
Multiple answers were allowed. Interviewer was instructed to not read a list of symptoms to the respondent.
Responses were categorized as listed.
Number and percent of respondents that agreed with the statement.
Most households agreed with statements about the rationale for community quarantine and expected behaviors of persons quarantined (eg, “quarantine can slow the spread of Ebola” [92%], and “I would follow my Town Chief’s directions about quarantine” [98%; Table 1]). More households in Villages A and B versus Villages C-G (63% vs 31%; χ2 P = .04) agreed that anyone who was told to stay in quarantine had the potential to acquire EVD, which might have been due to the CHT presence in Villages A and B, the EVD death, and the potential transmission within Village A. All (100%) respondents agreed that a person in a quarantined area deserved to have adequate water, food, and other basic needs, including going to clinics if they become ill.
Most (88%) residents of Villages A and B reported that the Margibi CHT explained “quarantine” to them, and of these households, all (100%) reported that they were given the opportunity to ask questions or share concerns before accepting the quarantine; the most common concern regarded the rationale and/or duration of quarantine (36%; Table 2). Most (56%) reported that someone from their household became sick or hurt during the quarantine; of these, all (100%) reported that they were able to go to a clinic, hospital, or ETU. One-half (50%) reported times when there was not enough water or food while they were quarantined. Most (81%) were frustrated to stay in quarantine, the most common reasons being unable to go to work/farm/school (38%) or to move about freely (31%).
Table 2.
Practices and Experiences during Quarantine, Villages A and B (N = 16), Margibi County, Liberia
| No. (%) | |
|---|---|
| The County Health Team and Others Explained Quarantine to Us: a | 14 (88) |
| I was given the opportunity to ask questions or share concerns before I accepted the quarantine (n = 14)a | 14 (100) |
| Questions and concerns about quarantine (n = 14)b | |
| Access to food/water | 4 (29) |
| How to prevent Ebola or what happens if someone in village becomes ill | 1 (7) |
| Rationale and duration of quarantine | 5 (36) |
| Needing to go to work, farm, or school | 3 (21) |
| Freedom of movement (other than needing to go to work, farm, school) | 1 (7) |
| Will quarantined persons be compensated? | 2 (14) |
| Did you stay in the village the entire time you were quarantined? | |
| Yes | 15 (94) |
| No | 1 (6) |
| Were you able to go to work while in quarantine? | |
| Yes | 1 (6) |
| No | 14 (88) |
| Don’t know | 1 (6) |
| Were you able to go to the market while in quarantine? | |
| Yes | 0 (0) |
| No | 16 (100) |
| Did anyone from your household get sick or hurt during quarantine? | |
| Yes | 9 (56) |
| Were they able to go to a clinic, hospital, or ETU? (n = 9) | |
| Yes | 9 (100) |
| Where did they go for treatment? (n = 9) | |
| Kakata ETU | 8 (89) |
| No answer recorded | 1 (11) |
| No | 7 (44) |
| Were there times when there wasn’t enough water or food while you were quarantined? | |
| Yes | 8 (50) |
| How often was there not enough water or food? (n = 8) | |
| Always | 1 (13) |
| Sometimes | 7 (88) |
| No | 8 (50) |
| Were you frustrated to have to stay in quarantine? | |
| Yes | 13 (81) |
| What frustrated you?b (n = 13) | |
| Unable to go to work/farm/school | 5 (38) |
| Unable to move about freely | 4 (31) |
| Needed access to food/water | 2 (15) |
| Fear/stigma of Ebola | 2 (15) |
| No | 3 (19) |
| Who did you tell if you had problems while under quarantine? No. (%) | |
| County Health Team | 13 (81) |
| Town Chief | 4 (25) |
| Partner Organization | 2 (13) |
| What did they do after you told them? No. (%) | |
| Provided food/water | 9 (56) |
| Nothing | 2 (13) |
| Provided psychosocial support | 1 (6) |
| Communicated our concerns to authorities | 0 (16) |
Abbreviation: ETU, Ebola treatment unit.
Number and percent of respondents that agreed with thestatement.
Multiple answers were allowed.
Discussion
Quarantine can be an effective method for preventing the spread of communicable diseases, and several communities in Liberia were subjected to quarantine during the epidemic as a method for preventing the further spread of EVD.6 The decision to quarantine must consider both the risk of transmission of EVD and the societal and economic costs,7 and failure to provide for residents’ basic needs can undermine a community quarantine.8–10 While the residents of the villages understood the importance of quarantine, most were also frustrated, for various reasons, to stay in quarantine. Like previous quarantines to prevent the spread of EVD,2,3 imposing the quarantine required substantial coordination between the Margibi CHT and emergency partners, staff time, and resources to both prevent spread of EVD outside of the affected villages and to meet the needs of the village residents.
This KAP assessment was performed retrospectively and it cannot be determined if or how monitoring/quarantine affected resident’s knowledge of EVD or attitudes about quarantine, or what unmet needs of residents existed before the quarantine. The fairly small number of households within this assessment precludes extensive statistical analysis, and the proportion of residents represented in these surveys could not be estimated for three villages. Respondent bias and interviewer bias are also possibilities, and the results presented here might not be generalizable outside of the surveyed communities.
Based on the findings presented here, health authorities might anticipate the need to:
Consider the health literacy of residents to ensure their understanding of the range of EVD known transmission routes, the EVD incubation period, and why the incubation period is crucial for determining the duration of monitoring or quarantine; and
Coordinate with partners to address the needs and concerns of quarantined persons (including access to water, food, and medical services), and actively work to meet these needs and address these concerns in order to maintain trust.
Conclusions
The community quarantine described here limited the spread of EVD. Residents understood the importance of monitoring and quarantine but had suboptimal knowledge of the routes of transmission and incubation period of EVD. One-half of quarantined households reported times of inadequate food and water, and most reported frustration with being in quarantine for various reasons; however, all household reporting injuries or illnesses while in quarantine received medical care.
Supplementary Material
Abbreviations:
- CDC
Centers for Disease Control and Prevention
- CHT
County Health Team
- ETU
Ebola treatment unit
- EVD
Ebola Virus Disease
- KAP
knowledge, attitudes, and practices
Footnotes
Conflicts of interest/disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention (Atlanta, Georgia USA). The authors declare no conflicts of interest.
Supplementary Material
To view supplementary material for this article, please visit https:/doi.org/10.1017/S1049023X17006720
References
- 1.Nyenswah T, Fallah M, Sieh S, et al. Controlling the last known cluster of Ebola Virus Disease – Liberia: January-February 2015. MMWR. 2015;64(18):500–504. [PMC free article] [PubMed] [Google Scholar]
- 2.Borchert M, Mutyaba I, Van Kerkhove MD, et al. Ebola hemorrhagic fever outbreak in Masindi District, Uganda: outbreak description and lessons learned. BMC Infect Dis. 2011;11:357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reaves EJ, Mabande LG, Thoroughman DA, Arwady MA, Montgomery JM. Control of Ebola virus disease - Firestone district, Liberia, 2014. MMWR. 2014;63(42):959–965. [PMC free article] [PubMed] [Google Scholar]
- 4.Dosso Z. Resentment simmers in Liberia’s “Ebola jail town.” Yahoo! News; September 7, 2014. [Google Scholar]
- 5.Onishi N. Quarantine for Ebola lifted in Liberia slum. New York Times. August 29, 2014. [Google Scholar]
- 6.Nyenswah T, Blackley DJ, Freeman T, et al. Community quarantine to interrupt Ebola virus transmission - Mawah Village, Bong County, Liberia, August-October, 2014. MMWR. 2015;64(7):179–182. [PMC free article] [PubMed] [Google Scholar]
- 7.Gostin LO. Public Health Law: Power, Duty, Restraint. Revision and expanded 2nd ed. Berkeley New York Milbank Memorial Fund: University of California Press; 2008. [Google Scholar]
- 8.Viens AM, Bensimon CM, Upshur REG. Your liberty or your life: reciprocity in the use of restrictive measures in contexts of contagion. J Bioetical Inq. 2009;6:207–217. [Google Scholar]
- 9.Eba PM. Ebola and human rights in West Africa. Lancet. 2014;384(9960):2091–2093. [DOI] [PubMed] [Google Scholar]
- 10.Thompson AK. Bioethics meets Ebola: exploring the moral landscape. British Medical Bulletin. 2016;117(1):5–13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


